The Gut-Brain Axis: How Leaky Gut and Leaky Brain Impact Your Health
The Gut-Brain Axis: How Leaky Gut and Leaky Brain Impact Your Health
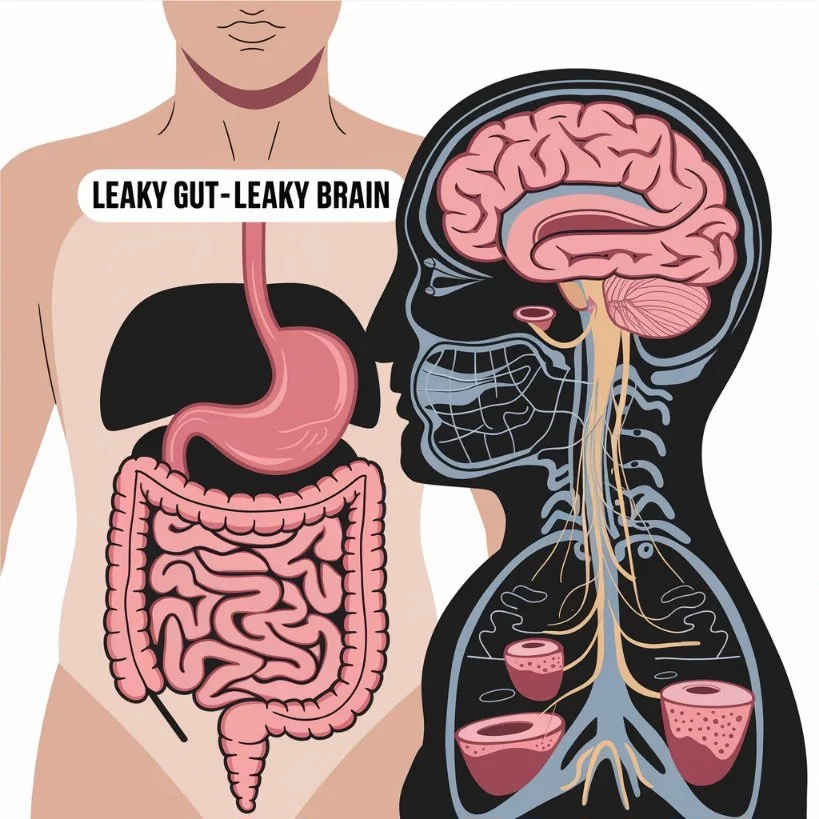
The saying “trust your gut” holds more truth than we may realize. Science has long recognized the connection between our digestive system and brain, a relationship known as the gut-brain axis. However, emerging research reveals that when this connection is compromised, it can lead to significant health challenges. One major contributor is the “leaky gut-leaky brain” phenomenon, a condition with profound effects on physical and mental health.
What Is Leaky Gut and Leaky Brain?
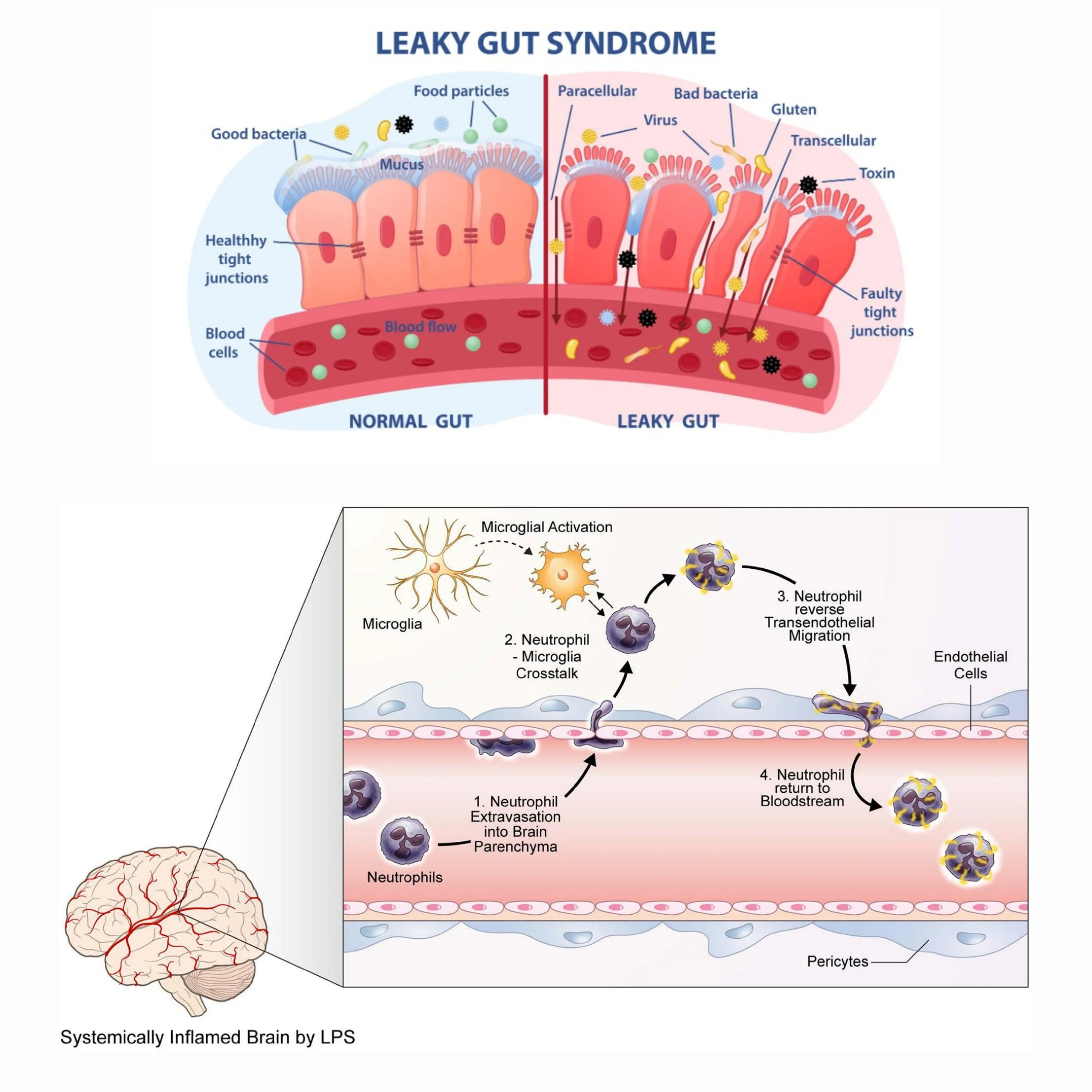
The gut lining acts as a selective barrier, allowing nutrients and beneficial compounds to pass into the bloodstream while keeping harmful substances like toxins, undigested food particles, and pathogens out. However, when this barrier becomes compromised—a condition known as leaky gut (or increased intestinal permeability)—these harmful substances escape into the bloodstream, triggering systemic inflammation.
At the same time, systemic inflammation caused by leaky gut can weaken the blood-brain barrier (BBB), which is the brain’s own protective shield. The BBB’s job is to block toxins, pathogens, and inflammatory molecules from entering the brain. When it becomes permeable (a condition often called "leaky brain"), harmful substances infiltrate the brain, leading to neuroinflammation and potentially damaging neurons and synaptic function.
Why a Healthy Gut-Brain Axis Is Crucial
A healthy gut-brain axis ensures effective communication between the gut and the brain, supporting physical and mental health. Disruption in this axis—caused by leaky gut and leaky brain—leads to a cascade of issues:
Neuroinflammation: Inflammatory cytokines from the gut travel to the brain, contributing to depression, anxiety, brain fog, and neurodegenerative diseases like Alzheimer’s.
Impaired Neurotransmitter Production: Gut dysbiosis reduces serotonin, dopamine, and GABA synthesis, affecting mood and cognitive function.
Hormonal Imbalances: Chronic gut inflammation can overstimulate the hypothalamic-pituitary-adrenal (HPA) axis, leading to cortisol dysregulation and worsening stress response.
Diseases and Autoimmune Disorders Linked to Gut-Brain Dysregulation
Some chronic conditions are particularly challenging because they inherently disrupt the gut-brain axis, making it difficult to achieve balance:
🌿 Celiac Disease
Celiac disease is an autoimmune disorder where gluten triggers an immune attack on the intestinal lining. This damage increases gut permeability, causing chronic inflammation and impairing nutrient absorption.
Studies have shown that individuals with celiac disease often experience anxiety, depression, and even neurological symptoms like brain fog due to the gut-brain axis disruption caused by gluten exposure.
🌿 Inflammatory Bowel Disease (IBD)
IBD, including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation and damage to the gut lining.
This inflammation can increase the permeability of both the gut and the BBB, leading to neuroinflammation and higher rates of anxiety and depression among patients with IBD.
🌿 Irritable Bowel Syndrome (IBS)
Although IBS is not an inflammatory condition, it is closely tied to dysbiosis and altered gut-brain communication.
People with IBS often report psychological symptoms like anxiety and depression, which are believed to result from imbalances in gut microbes affecting neurotransmitter production.
🌿 Autoimmune Encephalitis
In this condition, the immune system attacks the brain, often following a breach in the BBB caused by chronic inflammation or infection originating in the gut.
Symptoms include cognitive decline, mood disturbances, and even psychosis, underscoring the need for a healthy gut to protect brain health.
🌿 Multiple Sclerosis (MS)
MS is an autoimmune disease where the immune system attacks the protective covering of nerve fibers in the brain and spinal cord.
Research indicates a strong connection between gut microbiota imbalances and the onset or progression of MS, suggesting that gut dysbiosis and inflammation contribute to BBB dysfunction.
🌿 Autism Spectrum Disorders (ASD)
Many individuals with ASD exhibit signs of gut inflammation and dysbiosis, which may exacerbate neurological symptoms.
Gut-brain axis disruptions in ASD can affect brain development and contribute to behavioral challenges, underscoring the need for gut support in treatment plans.
Fun Fact:
Your gut contains over 100 million neurons, which is more than the number of neurons in your spinal cord. This is why the gut is often called the "second brain." In fact, these neurons in the gut produce 90% of the body's serotonin, the same neurotransmitter that influences mood and happiness! So, when your gut is happy, your brain has a much better chance of being happy too!
The Biological Cascade of Leaky Gut and Leaky Brain
🌿 Compromised Gut Lining (see graphics below)
Tight junctions in the intestinal lining become loose, allowing harmful substances to enter the bloodstream.
This triggers an immune response, increasing levels of inflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
🌿 Systemic Inflammation
These inflammatory markers travel throughout the body, damaging tissues, including the BBB.
🌿 Weakened Blood-Brain Barrier (see graphics below)
When the BBB becomes permeable, neurotoxins, pathogens, and inflammatory molecules infiltrate the brain.
Microglia, the brain’s immune cells, become activated, leading to chronic neuroinflammation.
🌿 Neurological and Psychological Symptoms
This inflammation impairs neuronal communication, reduces neuroplasticity, and disrupts neurotransmitter production, resulting in symptoms like brain fog, mood disorders, and cognitive decline.
By understanding and addressing the root causes of gut-brain axis disruption, including through diet, lifestyle changes, and targeted testing, we can restore this critical connection and improve overall health.
The Role of the Gut-Brain Axis in Mental Health
Your gut is often referred to as the "second brain," thanks to the vast network of neurons and nerve cells lining your gastrointestinal tract. This intricate system, called the enteric nervous system (ENS), is in constant communication with your central nervous system (CNS) via the vagus nerve. This bidirectional relationship forms the foundation of the gut-brain axis, influencing not only digestion but also mood, cognition, and emotional well-being.
The gut microbiome—the ecosystem of trillions of bacteria, fungi, and viruses residing in your digestive tract—plays a critical role in regulating this connection. Healthy microbiota help maintain the integrity of the gut lining, control inflammation, and synthesize essential neurotransmitters. However, when the gut-brain axis is disrupted, it can trigger or exacerbate a wide range of mental health challenges.
Mental Health Challenges Linked to Gut-Brain Dysregulation
🌿 Depression
Up to 90% of serotonin, the “feel-good” neurotransmitter, is produced in the gut. When the gut is inflamed or its microbial balance is disrupted, serotonin production decreases, contributing to low mood and depressive symptoms.
Inflammatory cytokines, often elevated due to gut permeability (leaky gut), can cross the blood-brain barrier and impair serotonin receptor function, exacerbating depression.
🌿 Anxiety
The gut produces gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter that calms the nervous system. Dysbiosis (an imbalance in gut microbes) can lead to reduced GABA levels, increasing feelings of stress and anxiety.
Studies show that gut inflammation can overstimulate the hypothalamic-pituitary-adrenal (HPA) axis, heightening the body’s stress response and fueling chronic anxiety.
🌿 Brain Fog and Cognitive Decline
Gut inflammation can lead to systemic inflammation, which impairs brain function by increasing oxidative stress and disrupting neuronal communication.
Toxins from a leaky gut may compromise the blood-brain barrier, allowing harmful substances to enter the brain and interfere with cognitive processes like memory and focus.
🌿 Chronic Fatigue Syndrome
A disrupted gut microbiome often leads to poor nutrient absorption, resulting in deficiencies in vitamins and minerals critical for energy production, such as B vitamins, magnesium, and iron.
Imbalanced gut bacteria can also produce excessive levels of lactic acid, which contributes to fatigue and low energy.
🌿 ADHD and Autism Spectrum Disorders (ASD)
Emerging research suggests that gut microbiota composition influences the development and severity of neurodevelopmental disorders.
Children with ADHD or ASD often show significant differences in their gut microbiome, including reduced microbial diversity and the presence of pro-inflammatory bacteria.
The Science Behind Gut-Brain Communication
Gut microbes produce a variety of metabolites that directly influence brain health:
Short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, derived from fiber fermentation, reduce inflammation and support brain function.
Lipopolysaccharides (LPS), produced by harmful bacteria, can increase neuroinflammation when the gut is imbalanced.
Tryptophan metabolism in the gut is essential for serotonin synthesis. A compromised gut may redirect tryptophan toward inflammatory pathways instead of serotonin production, reducing mood stability.
The Inflammatory Cycle
A leaky gut allows harmful substances, including undigested food particles and bacterial toxins, to enter the bloodstream. This triggers systemic inflammation, which can:
Cross the blood-brain barrier and inflame the brain.
Activate microglia (the brain’s immune cells), leading to a chronic inflammatory state associated with depression, anxiety, and cognitive decline.
In short, an unhealthy gut sets the stage for mental health challenges by disrupting neurotransmitter production, increasing inflammation, and impairing nutrient absorption. Healing the gut is a foundational step in improving mental well-being.
The Importance of Probiotics
Probiotics are live microorganisms that confer numerous health benefits when consumed in adequate amounts. These “good bacteria” play a vital role in maintaining gut health and, by extension, supporting the gut-brain axis. Here’s a deeper dive into how probiotics function, supported by science and biology:
🫴🏾 Reducing Inflammation
Mechanism: Probiotics modulate the immune system by increasing anti-inflammatory cytokines (e.g., interleukin-10) and reducing pro-inflammatory cytokines (e.g., interleukin-6 and TNF-α).
Impact on Gut and Brain: By reducing systemic inflammation, probiotics help protect the gut lining and the blood-brain barrier (BBB) from damage. For example:
Lactobacillus rhamnosus has been shown to reduce inflammation in the gut and lower neuroinflammation, alleviating symptoms of depression and anxiety.
Bifidobacterium breve decreases inflammation markers in individuals with inflammatory bowel disease (IBD).
🫴🏾 Supporting the Integrity of the Gut Lining
Mechanism: Probiotics enhance the production of mucin (a protective layer on the intestinal wall) and strengthen tight junction proteins, which hold the gut lining together.
Impact on Gut Permeability:
Probiotics prevent harmful substances like lipopolysaccharides (LPS) from passing through the gut lining into the bloodstream.
Strains like Saccharomyces boulardii and Bifidobacterium lactis have been shown to reduce gut permeability, effectively managing leaky gut.
Downstream Effects on the Brain: A healthy gut lining reduces systemic inflammation and protects the BBB, preventing neuroinflammation and associated symptoms like brain fog and mood disorders.
🫴🏾 Improving the Production of Brain-Friendly Neurotransmitters
Neurotransmitter Synthesis in the Gut:
Serotonin: Approximately 90% of the body's serotonin is produced in the gut by specific bacteria like Lactobacillus plantarum.
GABA: Probiotic strains like Lactobacillus rhamnosus enhance GABA production, calming the nervous system and reducing anxiety.
Dopamine: Some probiotics contribute to dopamine synthesis, improving motivation and focus.
Gut-Brain Communication via the Vagus Nerve: Probiotics influence the vagus nerve, the primary communication pathway between the gut and brain, to enhance mood and cognition.
🫴🏾 Balancing the Gut Microbiome
Dysbiosis Correction: Probiotics outcompete harmful bacteria and fungi, restoring a balanced microbiome. For example:
Bifidobacterium longum has been shown to reduce pathogenic overgrowths linked to gut-brain disruptions.
Lactobacillus casei supports a diverse microbial ecosystem, essential for neurotransmitter production and immune regulation.
Improved Short-Chain Fatty Acid (SCFA) Production:
SCFAs like butyrate, produced by probiotic fermentation of dietary fiber, reduce inflammation and protect both the gut and brain.
Butyrate also strengthens the BBB and supports neurogenesis (the growth of new brain cells).
Incorporating Probiotics for Gut-Brain Harmony
Adding probiotics to your daily routine is a powerful strategy for maintaining a healthy gut-brain axis. Here are some practical tips:
🌿 Probiotic-Rich Foods: Include fermented foods like yogurt, kefir, sauerkraut, kimchi, and tempeh.
🌿 Supplementation: Choose high-quality, multi-strain probiotic supplements containing strains like Lactobacillus rhamnosus, Bifidobacterium bifidum, and Saccharomyces boulardii.
🌿 Prebiotic Support: Feed your probiotics with prebiotic-rich foods such as bananas, garlic, onions, and asparagus to promote their growth and activity.
Why Probiotics Are a Game-Changer
By reducing inflammation, supporting gut integrity, and enhancing neurotransmitter production, probiotics restore harmony to the gut-brain axis. This can lead to significant improvements in mood, cognition, and overall health. A healthy gut microbiome, fortified with probiotics, acts as a powerful ally in protecting both the gut and brain from the effects of stress, poor diet, and environmental toxins.
Probiotics aren’t just about digestion—they’re integral to mental clarity, emotional resilience, and long-term health.
Why You Should Act Now
Your gut and brain are in constant communication, shaping every aspect of your health. Ignoring symptoms of gut imbalance can lead to chronic issues that diminish your quality of life. Whether you’re struggling with mental health concerns, unexplained fatigue, or digestive discomfort, addressing the gut-brain axis could be the breakthrough you need.
Ready to Take Control of Your Health?
At the heart of healing is understanding your body’s unique needs. As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I specialize in helping women like you restore vitality. Let’s uncover what’s holding you back with comprehensive testing and a personalized plan. Schedule your consultation today and start your journey toward optimal gut and brain health!
Your wellness starts here—don’t wait. The power to heal is within your grasp!
Creamy & Dreamy Plant-Based Probiotic Yogurt 🌱✨
Ingredients:
1. Luscious Base:
1 cup raw cashews or almonds (soaked overnight for ultimate creaminess 🥜)
OR 1 cup rich coconut milk for that tropical twist 🥥
2. Gut-Boosting Probiotic Starter:
1 capsule of probiotic supplement (vegan-friendly 🌱)
OR 2 tbsp store-bought plant-based yogurt with live cultures 🥄✨
3. Thick & Creamy Enhancers (Optional):
1 tsp agar-agar powder for a smooth, spoonable texture 🍶
OR 2 tbsp chia seeds for a nutrient-packed boost 🌟
4. Flavor Magic (Optional):
1 tsp vanilla extract (sweet and aromatic 🍦)
1 tbsp maple syrup or agave (a touch of natural sweetness 🍁)
5. Nutrient Powerhouse Add-Ons:
1 tsp inulin powder (feeds your good gut bacteria 🌾)
1 tbsp ground flaxseeds or hemp seeds for brain-boosting omega-3s 🌻
Instructions:
1. Blend the Creamy Base:
Drain and rinse soaked nuts (if using). Blend them with 1/2 cup water until ultra-smooth and velvety. Add more water for your desired consistency. 💧
2. Infuse with Probiotic Power:
Open the probiotic capsule and mix the powder gently into your yogurt base (don’t overheat—it’s alive! 🔥❌).
3. Thicken to Perfection:
Stir in agar-agar dissolved in warm water for a firm texture or mix chia seeds for a delightful crunch. Let sit for 10 minutes if using chia. 🧊
4. Magical Fermentation:
Pour your creamy mixture into a clean glass jar, cover lightly, and let it sit in a cozy spot for 8–12 hours. 🌡️
The result? A tangy, probiotic-rich dream that gets better the longer it ferments. 🕒
5. Chill & Devour:
Refrigerate for 2 hours to enhance its rich, tangy flavor. It’s now ready to wow your taste buds! 🍨✨
Serving Suggestions:
🍓 Top It Off: Add a handful of fresh berries (bursting with antioxidants), a sprinkle of granola for crunch, and a drizzle of golden honey.
🌰 Go Nutty: Sprinkle with chopped walnuts or pecans for an irresistible nutty finish.
🍫 Decadence Alert: Add a dusting of dark chocolate shavings or a dollop of almond butter.
Why You’ll Love It:
This yogurt isn’t just a treat—it’s a gut-brain connection booster! It’s creamy, tangy, and oh-so-satisfying. Dive in with a spoon and savor every velvety bite. 🥄💫 Your taste buds and tummy will thank you! 💕
References:
General Gut-Brain Axis
1. Mayer, E. A., Knight, R., Mazmanian, S. K., Cryan, J. F., & Tillisch, K. (2014). Gut microbes and the brain: Paradigm shift in neuroscience. The Journal of Neuroscience, 34(46), 15490–15496. https://doi.org/10.1523/JNEUROSCI.3299-14.2014
2. Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701–712. https://doi.org/10.1038/nrn3346
Leaky Gut and Leaky Brain
3. Fasano, A. (2012). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology, 42, 71–78. https://doi.org/10.1007/s12016-011-8291-x
4. Varatharaj, A., & Galea, I. (2017). The blood-brain barrier in systemic inflammation. Brain, Behavior, and Immunity, 60, 1–12. https://doi.org/10.1016/j.bbi.2016.03.010
Mental Health and Gut-Brain Axis
5. O'Mahony, S. M., Clarke, G., Borre, Y., Dinan, T. G., & Cryan, J. F. (2015). Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavioural Brain Research, 277, 32–48. https://doi.org/10.1016/j.bbr.2014.07.027
6. Foster, J. A., Rinaman, L., & Cryan, J. F. (2017). Stress & the gut-brain axis: Regulation by the microbiome. Neurobiology of Stress, 7, 124–136. https://doi.org/10.1016/j.ynstr.2017.03.001
Probiotics and Gut Health
7. Nagpal, R., & Yadav, H. (2017). Bacterial translocation from the gut to the distant organs: An overview. Annals of Nutrition & Metabolism, 71(Suppl. 1), 11–16. https://doi.org/10.1159/000479918
8. Liu, Y., & Alookaran, J. J. (2018). Probiotics in mental health. Frontiers in Psychiatry, 9, 671. https://doi.org/10.3389/fpsyt.2018.00671
9. Hemarajata, P., & Versalovic, J. (2013). Effects of probiotics on gut microbiota: Mechanisms of intestinal immunomodulation and neuromodulation. Therapeutic Advances in Gastroenterology, 6(1), 39–51. https://doi.org/10.1177/1756283X12459294
Diseases and Autoimmune Disorders
10. Ooi, C. Y., & Durie, P. R. (2012). Celiac disease and inflammatory bowel disease: Is there a connection? American Journal of Gastroenterology, 107(10), 1789–1794. https://doi.org/10.1038/ajg.2012.222
11. Peterson, C. T., Kumar, M., & Chauhan, A. (2018). Gut microbiome: A potential link to autism spectrum disorders. Frontiers in Cellular Neuroscience, 12, 528. https://doi.org/10.3389/fncel.2018.00528
12. Berer, K., Gerdes, L. A., Cekanaviciute, E., & Baranzini, S. E. (2017). Gut microbiome and multiple sclerosis: The role of short-chain fatty acids. Nature Communications, 8, 1077. https://pmc.ncbi.nlm.nih.gov/articles/PMC5730390/
Whole Food Diet and SCFAs
13. Koh, A., De Vadder, F., Kovatcheva-Datchary, P., & Bäckhed, F. (2016). From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell, 165(6), 1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
14. Graf, D., Di Cagno, R., Fåk, F., et al. (2015). Contribution of diet to the composition of the human gut microbiota. Microbial Ecology in Health and Disease, 26, 26164. https://doi.org/10.3402/mehd.v26.26164
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾