From Hormonal Chaos to Clarity: How Organizing Your Life Supports Your Health
From Hormonal Chaos to Clarity: How Organizing Your Life Supports Your Health
Have you ever felt like your mind is constantly cluttered, you can’t focus, and no matter how hard you try, you just can’t seem to get organized? If you’re a woman navigating perimenopause or hormonal changes, you’re not imagining things—your brain is actually changing.
Many women experience brain fog, forgetfulness, and a sense of feeling scattered during this transition. The good news? There are ways to regain clarity and structure in your life. Organizing your thoughts, tasks, and goals isn’t just about productivity—it’s a key part of supporting your mental and physical well-being.
That’s why I’m thrilled to introduce Organise My Dreams, a trusted partner dedicated to helping women bring order to their lives, rediscover their purpose, and move forward with confidence.
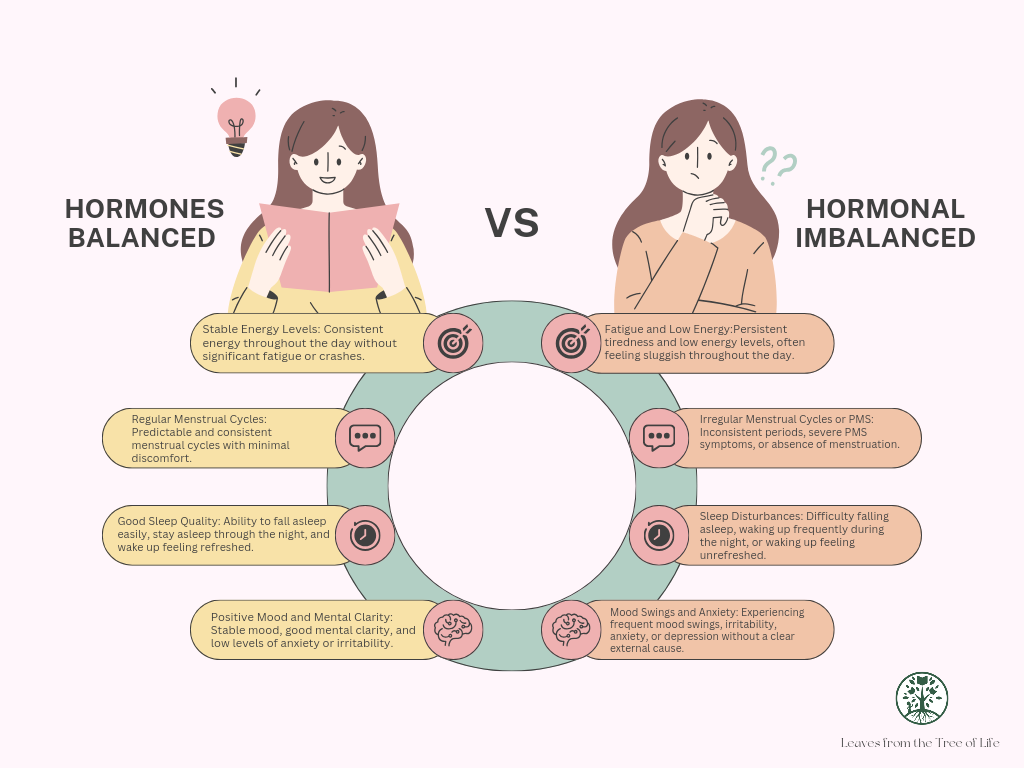
Why Hormonal Changes Can Make You Feel Disorganized
Hormonal shifts, particularly in midlife, significantly impact how a woman thinks, feels, and processes information.
🌿 Estrogen & Cognitive Function: Estrogen plays a vital role in brain function, including memory, focus, and mental clarity. As estrogen fluctuates and declines during perimenopause and menopause, many women report difficulty concentrating, increased forgetfulness, and mental fog.
🌿 Cortisol & Stress Response: When estrogen drops, cortisol (the stress hormone) can become imbalanced, making women more prone to overwhelm, anxiety, and difficulty managing daily tasks.
🌿 Brain Shrinkage During Menopause: A study in Neurology found that women's brains can lose up to 2% of their volume during the menopausal transition, particularly in areas linked to memory and organization. The good news? Brain function often recovers post-menopause, but in the meantime, support is crucial.
🌿 The Multitasking Myth: Research shows that women, especially during hormonal transitions, struggle with multitasking more than they realize. When the brain is under stress, juggling multiple responsibilities can lead to even greater disorganization and frustration.
The Power of Organization for Mental Clarity
When your mind feels cluttered, your life can feel chaotic. That’s why having structure, routines, and clear goals can be a game-changer for women in transition.
Creating daily routines reduces stress and improves focus.
Setting clear goals helps your brain prioritize and function more efficiently.
Organizing your physical and digital space can improve mental clarity and reduce overwhelm.
But let’s be honest—sometimes, it’s hard to do this on your own. That’s where Organise My Dreams comes in.
Fun Fact:
Did you know that women’s brains become more energy-efficient after menopause?
While hormonal shifts can cause temporary brain fog and forgetfulness, research from the University of California, Berkeley, found that women's brains actually adapt and become more efficient post-menopause. This means that even though the transition can feel overwhelming, your brain is working to rewire itself for a new phase of clarity and focus.
So, if you’re feeling scattered now, take heart—with the right support and organization, you can come out on the other side sharper and more in control than ever!
How Organise My Dreams Can Help You Take Control
Organise My Dreams is designed for women who feel overwhelmed, lost, or unsure about their next steps. Their services help bring structure and purpose back into your life so you can move forward with confidence.
They specialize in:
✅ Goal Setting & Planning – Helping you identify what truly matters and break it down into manageable steps.
✅ Time & Task Management – Teaching strategies to help you stay on top of responsibilities without feeling stressed.
✅ Mindset & Motivation – Supporting you in shifting from feeling stuck to feeling empowered.
✅ Life Organization Tools – Providing practical systems to keep your life in order.
Imagine waking up every day feeling clear, focused, and in control—knowing exactly what you need to do and feeling confident in your ability to do it. That’s what Organise My Dreams can help you achieve.
Your Health and Dreams Go Hand in Hand
At Leaves from the Tree of Life LLC, I focus on helping women achieve optimal health through functional nutrition, gut health support, and hormonal balance. But true wellness isn’t just about diet and supplements—it’s about mental clarity, purpose, and emotional well-being.
Having a clear vision for your life and an organized mind can reduce stress, support better decision-making, and even help balance your hormones. That’s why I encourage my clients to take control of both their health and their life structure.
Take the Next Step Toward Clarity
If you’re struggling with brain fog, stress, or feeling unorganized due to hormonal changes, now is the time to take action.
✨ If you need support with your health and well-being, reach out to me at Leaves from the Tree of Life LLC—I’ll help you regain your vitality and balance.
✨ If you’re looking for expert guidance on organizing your life and creating a structured, fulfilling future, I highly recommend connecting with Organise My Dreams.
Your dreams, goals, and well-being are worth investing in. Don’t let disorganization and overwhelm hold you back—take the first step today!
Golden Glow Stuffed Sweet Peppers with Creamy Turmeric Tahini Drizzle ✨🫑
These Golden Glow Stuffed Sweet Peppers are a flavorful, nutrient-packed meal featuring roasted bell peppers filled with a hearty mix of quinoa, chickpeas, sun-dried tomatoes, roasted cauliflower pearls, and toasted pumpkin seeds, all tossed in a citrus-herb dressing. A creamy turmeric tahini drizzle ties everything together, making each bite irresistibly delicious and nourishing! 🌿✨
🌟 Ingredients
For the Stuffed Peppers:
4 large sweet bell peppers (red, yellow, or orange)
1 cup quinoa, rinsed and cooked
1 can (15 oz) chickpeas, drained and rinsed
1 cup roasted cauliflower pearls (bite-sized pieces roasted until golden)
½ cup sun-dried tomatoes, chopped
¼ cup toasted pumpkin seeds
2 tbsp fresh parsley, chopped
2 tbsp fresh mint, chopped
Zest of 1 lemon
For the Citrus-Herb Dressing:
3 tbsp olive oil
Juice of 1 lemon
1 tbsp apple cider vinegar
1 tsp Dijon mustard
1 clove garlic, minced
½ tsp sea salt
¼ tsp black pepper
For the Creamy Turmeric Tahini Drizzle:
¼ cup tahini
2 tbsp lemon juice
½ tsp turmeric powder
1 clove garlic, minced
1 tbsp maple syrup
2-3 tbsp water (adjust for desired consistency)
¼ tsp sea salt
🥄 How to Make It
Step 1: Roast the Peppers
1. Preheat your oven to 400°F (200°C).
2. Slice the tops off the bell peppers and remove the seeds. Lightly brush them with olive oil.
3. Place them on a baking sheet, cut side up, and roast for 15-20 minutes, until slightly charred and softened.
Step 2: Prepare the Filling
1. Cook the quinoa according to package instructions and let it cool slightly.
2. In a large bowl, combine the cooked quinoa, chickpeas, roasted cauliflower pearls, sun-dried tomatoes, pumpkin seeds, parsley, mint, and lemon zest.
Step 3: Make the Citrus-Herb Dressing
1. In a small bowl, whisk together the olive oil, lemon juice, apple cider vinegar, Dijon mustard, minced garlic, salt, and black pepper.
2. Pour over the quinoa mixture and toss until well combined.
Step 4: Make the Creamy Turmeric Tahini Drizzle
1. In a small bowl, whisk together tahini, lemon juice, turmeric, garlic, maple syrup, salt, and water until smooth and creamy. Adjust water for desired consistency.
Step 5: Assemble & Serve
1. Spoon the quinoa filling into the roasted bell peppers.
2. Drizzle generously with the creamy turmeric tahini sauce.
3. Garnish with additional fresh herbs and a sprinkle of pumpkin seeds for extra crunch!
🔥 Health Benefits of Key Ingredients:
✅ Turmeric 🧡 – A powerful anti-inflammatory spice that supports brain health and hormone balance.
✅ Chickpeas 🥣 – High in plant-based protein and fiber, helping to regulate digestion and blood sugar.
✅ Pumpkin Seeds 🎃 – Rich in magnesium and zinc, supporting relaxation and hormonal health.
✅ Sun-Dried Tomatoes 🍅 – Loaded with antioxidants like lycopene, promoting skin health and reducing oxidative stress.
This Golden Glow Stuffed Sweet Peppers dish is not just visually stunning—it’s a celebration of whole food flavors that nourish your mind and body! 🌿✨ Enjoy this delicious plant-based meal and feel the glow from the inside out! 🌞💛
Citations
https://news.weill.cornell.edu/news/2021/06/imaging-study-reveals-brain-changes-during-the-transition-to-menopause
https://pmc.ncbi.nlm.nih.gov/articles/PMC8190071/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4838456/
https://pmc.ncbi.nlm.nih.gov/articles/PMC10561270/
https://academic.oup.com/edrv/article-abstract/24/2/133/2424179?redirectedFrom=fulltext
https://lonestarneurology.net/others/understanding-the-impact-of-hormonal-changes-on-neurological-function/
https://cibs.uahs.arizona.edu/2023/05/31/how-menopause-reshapes-the-brain/
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
The Gut-Brain Axis: How Leaky Gut and Leaky Brain Impact Your Health
The Gut-Brain Axis: How Leaky Gut and Leaky Brain Impact Your Health
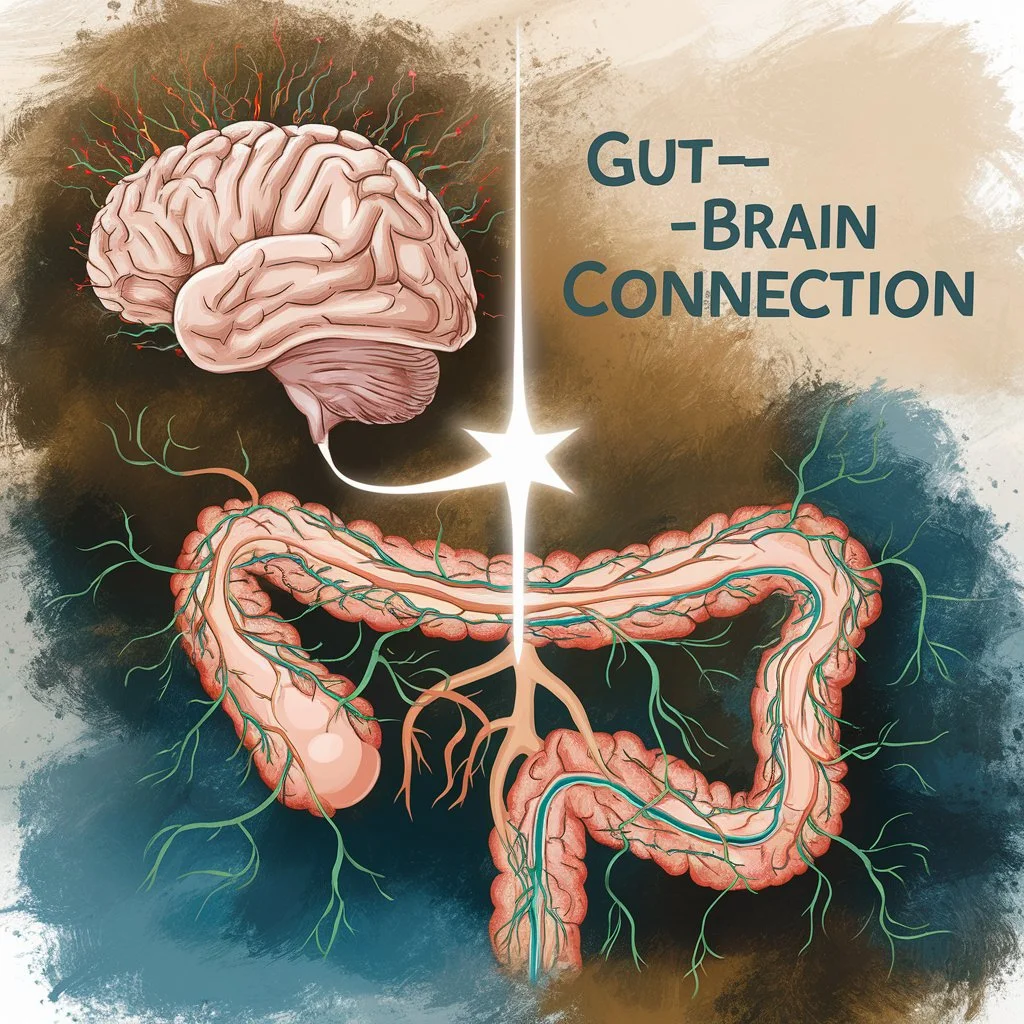
The saying “trust your gut” holds more truth than we may realize. Science has long recognized the connection between our digestive system and brain, a relationship known as the gut-brain axis. However, emerging research reveals that when this connection is compromised, it can lead to significant health challenges. One major contributor is the “leaky gut-leaky brain” phenomenon, a condition with profound effects on physical and mental health.
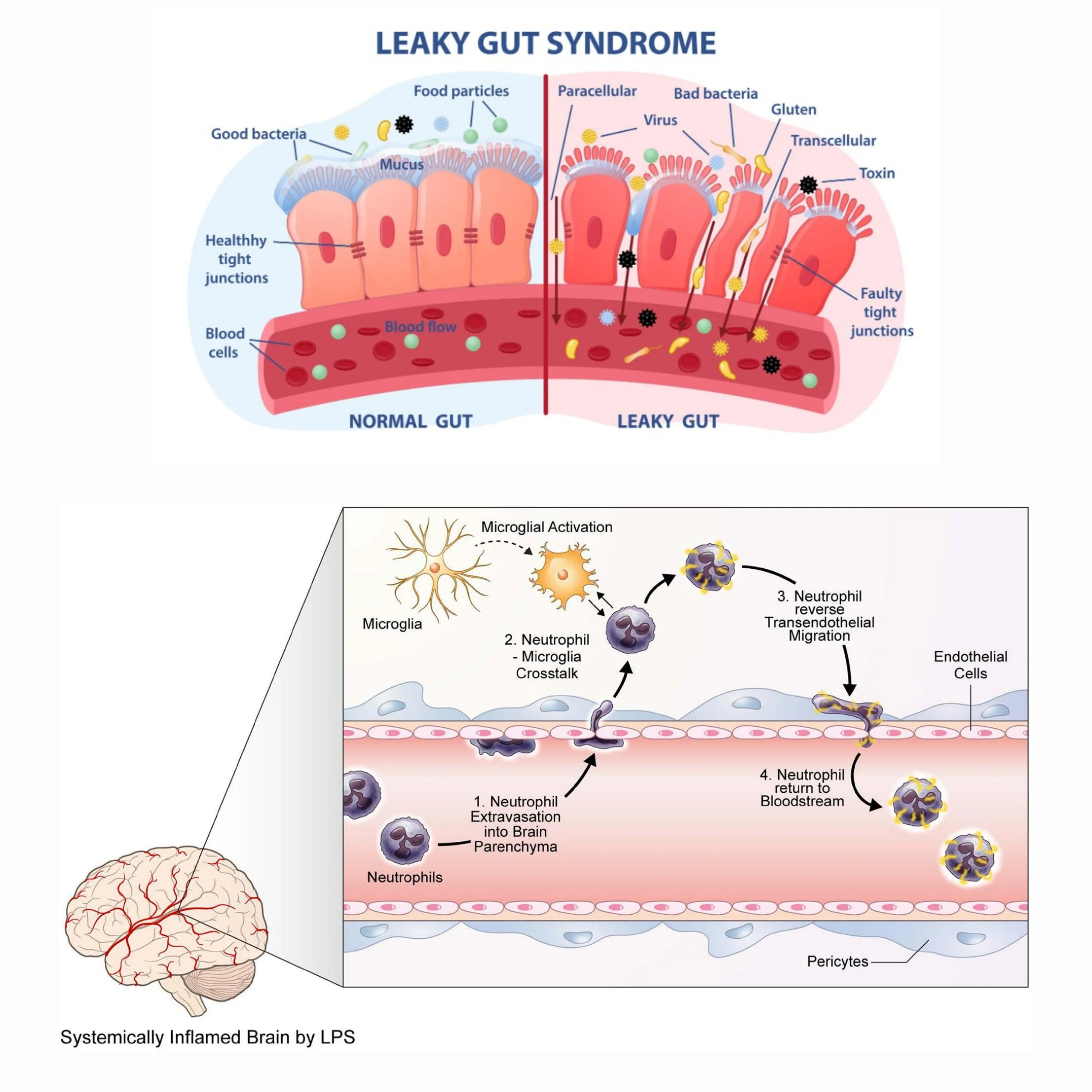
What Is Leaky Gut and Leaky Brain?
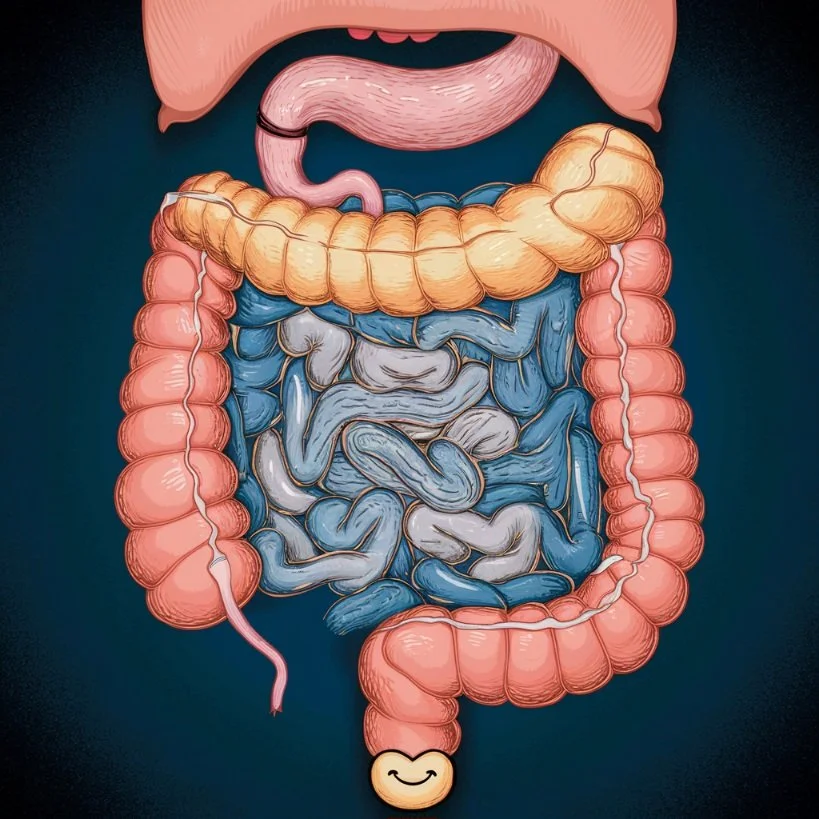
The gut lining acts as a selective barrier, allowing nutrients and beneficial compounds to pass into the bloodstream while keeping harmful substances like toxins, undigested food particles, and pathogens out. However, when this barrier becomes compromised—a condition known as leaky gut (or increased intestinal permeability)—these harmful substances escape into the bloodstream, triggering systemic inflammation.
At the same time, systemic inflammation caused by leaky gut can weaken the blood-brain barrier (BBB), which is the brain’s own protective shield. The BBB’s job is to block toxins, pathogens, and inflammatory molecules from entering the brain. When it becomes permeable (a condition often called "leaky brain"), harmful substances infiltrate the brain, leading to neuroinflammation and potentially damaging neurons and synaptic function.
Why a Healthy Gut-Brain Axis Is Crucial
A healthy gut-brain axis ensures effective communication between the gut and the brain, supporting physical and mental health. Disruption in this axis—caused by leaky gut and leaky brain—leads to a cascade of issues:
Neuroinflammation: Inflammatory cytokines from the gut travel to the brain, contributing to depression, anxiety, brain fog, and neurodegenerative diseases like Alzheimer’s.
Impaired Neurotransmitter Production: Gut dysbiosis reduces serotonin, dopamine, and GABA synthesis, affecting mood and cognitive function.
Hormonal Imbalances: Chronic gut inflammation can overstimulate the hypothalamic-pituitary-adrenal (HPA) axis, leading to cortisol dysregulation and worsening stress response.
Diseases and Autoimmune Disorders Linked to Gut-Brain Dysregulation
Some chronic conditions are particularly challenging because they inherently disrupt the gut-brain axis, making it difficult to achieve balance:
🌿 Celiac Disease
Celiac disease is an autoimmune disorder where gluten triggers an immune attack on the intestinal lining. This damage increases gut permeability, causing chronic inflammation and impairing nutrient absorption.
Studies have shown that individuals with celiac disease often experience anxiety, depression, and even neurological symptoms like brain fog due to the gut-brain axis disruption caused by gluten exposure.
🌿 Inflammatory Bowel Disease (IBD)
IBD, including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation and damage to the gut lining.
This inflammation can increase the permeability of both the gut and the BBB, leading to neuroinflammation and higher rates of anxiety and depression among patients with IBD.
🌿 Irritable Bowel Syndrome (IBS)
Although IBS is not an inflammatory condition, it is closely tied to dysbiosis and altered gut-brain communication.
People with IBS often report psychological symptoms like anxiety and depression, which are believed to result from imbalances in gut microbes affecting neurotransmitter production.
🌿 Autoimmune Encephalitis
In this condition, the immune system attacks the brain, often following a breach in the BBB caused by chronic inflammation or infection originating in the gut.
Symptoms include cognitive decline, mood disturbances, and even psychosis, underscoring the need for a healthy gut to protect brain health.
🌿 Multiple Sclerosis (MS)
MS is an autoimmune disease where the immune system attacks the protective covering of nerve fibers in the brain and spinal cord.
Research indicates a strong connection between gut microbiota imbalances and the onset or progression of MS, suggesting that gut dysbiosis and inflammation contribute to BBB dysfunction.
🌿 Autism Spectrum Disorders (ASD)
Many individuals with ASD exhibit signs of gut inflammation and dysbiosis, which may exacerbate neurological symptoms.
Gut-brain axis disruptions in ASD can affect brain development and contribute to behavioral challenges, underscoring the need for gut support in treatment plans.
Fun Fact:
Your gut contains over 100 million neurons, which is more than the number of neurons in your spinal cord. This is why the gut is often called the "second brain." In fact, these neurons in the gut produce 90% of the body's serotonin, the same neurotransmitter that influences mood and happiness! So, when your gut is happy, your brain has a much better chance of being happy too!
The Biological Cascade of Leaky Gut and Leaky Brain
🌿 Compromised Gut Lining (see graphics below)
Tight junctions in the intestinal lining become loose, allowing harmful substances to enter the bloodstream.
This triggers an immune response, increasing levels of inflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
🌿 Systemic Inflammation
These inflammatory markers travel throughout the body, damaging tissues, including the BBB.
🌿 Weakened Blood-Brain Barrier (see graphics below)
When the BBB becomes permeable, neurotoxins, pathogens, and inflammatory molecules infiltrate the brain.
Microglia, the brain’s immune cells, become activated, leading to chronic neuroinflammation.
🌿 Neurological and Psychological Symptoms
This inflammation impairs neuronal communication, reduces neuroplasticity, and disrupts neurotransmitter production, resulting in symptoms like brain fog, mood disorders, and cognitive decline.
By understanding and addressing the root causes of gut-brain axis disruption, including through diet, lifestyle changes, and targeted testing, we can restore this critical connection and improve overall health.
The Role of the Gut-Brain Axis in Mental Health
Your gut is often referred to as the "second brain," thanks to the vast network of neurons and nerve cells lining your gastrointestinal tract. This intricate system, called the enteric nervous system (ENS), is in constant communication with your central nervous system (CNS) via the vagus nerve. This bidirectional relationship forms the foundation of the gut-brain axis, influencing not only digestion but also mood, cognition, and emotional well-being.
The gut microbiome—the ecosystem of trillions of bacteria, fungi, and viruses residing in your digestive tract—plays a critical role in regulating this connection. Healthy microbiota help maintain the integrity of the gut lining, control inflammation, and synthesize essential neurotransmitters. However, when the gut-brain axis is disrupted, it can trigger or exacerbate a wide range of mental health challenges.
Mental Health Challenges Linked to Gut-Brain Dysregulation
🌿 Depression
Up to 90% of serotonin, the “feel-good” neurotransmitter, is produced in the gut. When the gut is inflamed or its microbial balance is disrupted, serotonin production decreases, contributing to low mood and depressive symptoms.
Inflammatory cytokines, often elevated due to gut permeability (leaky gut), can cross the blood-brain barrier and impair serotonin receptor function, exacerbating depression.
🌿 Anxiety
The gut produces gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter that calms the nervous system. Dysbiosis (an imbalance in gut microbes) can lead to reduced GABA levels, increasing feelings of stress and anxiety.
Studies show that gut inflammation can overstimulate the hypothalamic-pituitary-adrenal (HPA) axis, heightening the body’s stress response and fueling chronic anxiety.
🌿 Brain Fog and Cognitive Decline
Gut inflammation can lead to systemic inflammation, which impairs brain function by increasing oxidative stress and disrupting neuronal communication.
Toxins from a leaky gut may compromise the blood-brain barrier, allowing harmful substances to enter the brain and interfere with cognitive processes like memory and focus.
🌿 Chronic Fatigue Syndrome
A disrupted gut microbiome often leads to poor nutrient absorption, resulting in deficiencies in vitamins and minerals critical for energy production, such as B vitamins, magnesium, and iron.
Imbalanced gut bacteria can also produce excessive levels of lactic acid, which contributes to fatigue and low energy.
🌿 ADHD and Autism Spectrum Disorders (ASD)
Emerging research suggests that gut microbiota composition influences the development and severity of neurodevelopmental disorders.
Children with ADHD or ASD often show significant differences in their gut microbiome, including reduced microbial diversity and the presence of pro-inflammatory bacteria.
The Science Behind Gut-Brain Communication
Gut microbes produce a variety of metabolites that directly influence brain health:
Short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, derived from fiber fermentation, reduce inflammation and support brain function.
Lipopolysaccharides (LPS), produced by harmful bacteria, can increase neuroinflammation when the gut is imbalanced.
Tryptophan metabolism in the gut is essential for serotonin synthesis. A compromised gut may redirect tryptophan toward inflammatory pathways instead of serotonin production, reducing mood stability.
The Inflammatory Cycle
A leaky gut allows harmful substances, including undigested food particles and bacterial toxins, to enter the bloodstream. This triggers systemic inflammation, which can:
Cross the blood-brain barrier and inflame the brain.
Activate microglia (the brain’s immune cells), leading to a chronic inflammatory state associated with depression, anxiety, and cognitive decline.
In short, an unhealthy gut sets the stage for mental health challenges by disrupting neurotransmitter production, increasing inflammation, and impairing nutrient absorption. Healing the gut is a foundational step in improving mental well-being.
The Importance of Probiotics
Probiotics are live microorganisms that confer numerous health benefits when consumed in adequate amounts. These “good bacteria” play a vital role in maintaining gut health and, by extension, supporting the gut-brain axis. Here’s a deeper dive into how probiotics function, supported by science and biology:
🫴🏾 Reducing Inflammation
Mechanism: Probiotics modulate the immune system by increasing anti-inflammatory cytokines (e.g., interleukin-10) and reducing pro-inflammatory cytokines (e.g., interleukin-6 and TNF-α).
Impact on Gut and Brain: By reducing systemic inflammation, probiotics help protect the gut lining and the blood-brain barrier (BBB) from damage. For example:
Lactobacillus rhamnosus has been shown to reduce inflammation in the gut and lower neuroinflammation, alleviating symptoms of depression and anxiety.
Bifidobacterium breve decreases inflammation markers in individuals with inflammatory bowel disease (IBD).
🫴🏾 Supporting the Integrity of the Gut Lining
Mechanism: Probiotics enhance the production of mucin (a protective layer on the intestinal wall) and strengthen tight junction proteins, which hold the gut lining together.
Impact on Gut Permeability:
Probiotics prevent harmful substances like lipopolysaccharides (LPS) from passing through the gut lining into the bloodstream.
Strains like Saccharomyces boulardii and Bifidobacterium lactis have been shown to reduce gut permeability, effectively managing leaky gut.
Downstream Effects on the Brain: A healthy gut lining reduces systemic inflammation and protects the BBB, preventing neuroinflammation and associated symptoms like brain fog and mood disorders.
🫴🏾 Improving the Production of Brain-Friendly Neurotransmitters
Neurotransmitter Synthesis in the Gut:
Serotonin: Approximately 90% of the body's serotonin is produced in the gut by specific bacteria like Lactobacillus plantarum.
GABA: Probiotic strains like Lactobacillus rhamnosus enhance GABA production, calming the nervous system and reducing anxiety.
Dopamine: Some probiotics contribute to dopamine synthesis, improving motivation and focus.
Gut-Brain Communication via the Vagus Nerve: Probiotics influence the vagus nerve, the primary communication pathway between the gut and brain, to enhance mood and cognition.
🫴🏾 Balancing the Gut Microbiome
Dysbiosis Correction: Probiotics outcompete harmful bacteria and fungi, restoring a balanced microbiome. For example:
Bifidobacterium longum has been shown to reduce pathogenic overgrowths linked to gut-brain disruptions.
Lactobacillus casei supports a diverse microbial ecosystem, essential for neurotransmitter production and immune regulation.
Improved Short-Chain Fatty Acid (SCFA) Production:
SCFAs like butyrate, produced by probiotic fermentation of dietary fiber, reduce inflammation and protect both the gut and brain.
Butyrate also strengthens the BBB and supports neurogenesis (the growth of new brain cells).
Incorporating Probiotics for Gut-Brain Harmony
Adding probiotics to your daily routine is a powerful strategy for maintaining a healthy gut-brain axis. Here are some practical tips:
🌿 Probiotic-Rich Foods: Include fermented foods like yogurt, kefir, sauerkraut, kimchi, and tempeh.
🌿 Supplementation: Choose high-quality, multi-strain probiotic supplements containing strains like Lactobacillus rhamnosus, Bifidobacterium bifidum, and Saccharomyces boulardii.
🌿 Prebiotic Support: Feed your probiotics with prebiotic-rich foods such as bananas, garlic, onions, and asparagus to promote their growth and activity.
Why Probiotics Are a Game-Changer
By reducing inflammation, supporting gut integrity, and enhancing neurotransmitter production, probiotics restore harmony to the gut-brain axis. This can lead to significant improvements in mood, cognition, and overall health. A healthy gut microbiome, fortified with probiotics, acts as a powerful ally in protecting both the gut and brain from the effects of stress, poor diet, and environmental toxins.
Probiotics aren’t just about digestion—they’re integral to mental clarity, emotional resilience, and long-term health.
Why You Should Act Now
Your gut and brain are in constant communication, shaping every aspect of your health. Ignoring symptoms of gut imbalance can lead to chronic issues that diminish your quality of life. Whether you’re struggling with mental health concerns, unexplained fatigue, or digestive discomfort, addressing the gut-brain axis could be the breakthrough you need.
Ready to Take Control of Your Health?
At the heart of healing is understanding your body’s unique needs. As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I specialize in helping women like you restore vitality. Let’s uncover what’s holding you back with comprehensive testing and a personalized plan. Schedule your consultation today and start your journey toward optimal gut and brain health!
Your wellness starts here—don’t wait. The power to heal is within your grasp!
Creamy & Dreamy Plant-Based Probiotic Yogurt 🌱✨
Ingredients:
1. Luscious Base:
1 cup raw cashews or almonds (soaked overnight for ultimate creaminess 🥜)
OR 1 cup rich coconut milk for that tropical twist 🥥
2. Gut-Boosting Probiotic Starter:
1 capsule of probiotic supplement (vegan-friendly 🌱)
OR 2 tbsp store-bought plant-based yogurt with live cultures 🥄✨
3. Thick & Creamy Enhancers (Optional):
1 tsp agar-agar powder for a smooth, spoonable texture 🍶
OR 2 tbsp chia seeds for a nutrient-packed boost 🌟
4. Flavor Magic (Optional):
1 tsp vanilla extract (sweet and aromatic 🍦)
1 tbsp maple syrup or agave (a touch of natural sweetness 🍁)
5. Nutrient Powerhouse Add-Ons:
1 tsp inulin powder (feeds your good gut bacteria 🌾)
1 tbsp ground flaxseeds or hemp seeds for brain-boosting omega-3s 🌻
Instructions:
1. Blend the Creamy Base:
Drain and rinse soaked nuts (if using). Blend them with 1/2 cup water until ultra-smooth and velvety. Add more water for your desired consistency. 💧
2. Infuse with Probiotic Power:
Open the probiotic capsule and mix the powder gently into your yogurt base (don’t overheat—it’s alive! 🔥❌).
3. Thicken to Perfection:
Stir in agar-agar dissolved in warm water for a firm texture or mix chia seeds for a delightful crunch. Let sit for 10 minutes if using chia. 🧊
4. Magical Fermentation:
Pour your creamy mixture into a clean glass jar, cover lightly, and let it sit in a cozy spot for 8–12 hours. 🌡️
The result? A tangy, probiotic-rich dream that gets better the longer it ferments. 🕒
5. Chill & Devour:
Refrigerate for 2 hours to enhance its rich, tangy flavor. It’s now ready to wow your taste buds! 🍨✨
Serving Suggestions:
🍓 Top It Off: Add a handful of fresh berries (bursting with antioxidants), a sprinkle of granola for crunch, and a drizzle of golden honey.
🌰 Go Nutty: Sprinkle with chopped walnuts or pecans for an irresistible nutty finish.
🍫 Decadence Alert: Add a dusting of dark chocolate shavings or a dollop of almond butter.
Why You’ll Love It:
This yogurt isn’t just a treat—it’s a gut-brain connection booster! It’s creamy, tangy, and oh-so-satisfying. Dive in with a spoon and savor every velvety bite. 🥄💫 Your taste buds and tummy will thank you! 💕
References:
General Gut-Brain Axis
1. Mayer, E. A., Knight, R., Mazmanian, S. K., Cryan, J. F., & Tillisch, K. (2014). Gut microbes and the brain: Paradigm shift in neuroscience. The Journal of Neuroscience, 34(46), 15490–15496. https://doi.org/10.1523/JNEUROSCI.3299-14.2014
2. Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701–712. https://doi.org/10.1038/nrn3346
Leaky Gut and Leaky Brain
3. Fasano, A. (2012). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology, 42, 71–78. https://doi.org/10.1007/s12016-011-8291-x
4. Varatharaj, A., & Galea, I. (2017). The blood-brain barrier in systemic inflammation. Brain, Behavior, and Immunity, 60, 1–12. https://doi.org/10.1016/j.bbi.2016.03.010
Mental Health and Gut-Brain Axis
5. O'Mahony, S. M., Clarke, G., Borre, Y., Dinan, T. G., & Cryan, J. F. (2015). Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavioural Brain Research, 277, 32–48. https://doi.org/10.1016/j.bbr.2014.07.027
6. Foster, J. A., Rinaman, L., & Cryan, J. F. (2017). Stress & the gut-brain axis: Regulation by the microbiome. Neurobiology of Stress, 7, 124–136. https://doi.org/10.1016/j.ynstr.2017.03.001
Probiotics and Gut Health
7. Nagpal, R., & Yadav, H. (2017). Bacterial translocation from the gut to the distant organs: An overview. Annals of Nutrition & Metabolism, 71(Suppl. 1), 11–16. https://doi.org/10.1159/000479918
8. Liu, Y., & Alookaran, J. J. (2018). Probiotics in mental health. Frontiers in Psychiatry, 9, 671. https://doi.org/10.3389/fpsyt.2018.00671
9. Hemarajata, P., & Versalovic, J. (2013). Effects of probiotics on gut microbiota: Mechanisms of intestinal immunomodulation and neuromodulation. Therapeutic Advances in Gastroenterology, 6(1), 39–51. https://doi.org/10.1177/1756283X12459294
Diseases and Autoimmune Disorders
10. Ooi, C. Y., & Durie, P. R. (2012). Celiac disease and inflammatory bowel disease: Is there a connection? American Journal of Gastroenterology, 107(10), 1789–1794. https://doi.org/10.1038/ajg.2012.222
11. Peterson, C. T., Kumar, M., & Chauhan, A. (2018). Gut microbiome: A potential link to autism spectrum disorders. Frontiers in Cellular Neuroscience, 12, 528. https://doi.org/10.3389/fncel.2018.00528
12. Berer, K., Gerdes, L. A., Cekanaviciute, E., & Baranzini, S. E. (2017). Gut microbiome and multiple sclerosis: The role of short-chain fatty acids. Nature Communications, 8, 1077. https://pmc.ncbi.nlm.nih.gov/articles/PMC5730390/
Whole Food Diet and SCFAs
13. Koh, A., De Vadder, F., Kovatcheva-Datchary, P., & Bäckhed, F. (2016). From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell, 165(6), 1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
14. Graf, D., Di Cagno, R., Fåk, F., et al. (2015). Contribution of diet to the composition of the human gut microbiota. Microbial Ecology in Health and Disease, 26, 26164. https://doi.org/10.3402/mehd.v26.26164
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Understanding Anemia: Root Causes, Types, and How to Reclaim Vitality
Understanding Anemia: Root Causes, Types, and How to Reclaim Vitality
Anemia is a common yet often misunderstood condition that affects millions worldwide. Its symptoms—fatigue, weakness, and pale skin—can significantly impact quality of life. However, anemia is not just about low iron; it’s a sign of deeper imbalances in the body. This article explores the various types of anemia, the root causes, and how factors like parasitic infections and low stomach acid create a fertile ground for anemia to thrive. Let’s dig into how to identify and address anemia to restore vitality and health.
What Is Anemia?
Anemia occurs when the body doesn’t have enough healthy red blood cells or hemoglobin to carry oxygen to tissues, leaving you fatigued and weak. While iron deficiency anemia is the most well-known type, anemia comes in different forms with various underlying causes.
Types of Anemia
Iron Deficiency Anemia
Caused by inadequate dietary iron intake, blood loss, or poor absorption.
Vitamin B12 Deficiency Anemia (Pernicious Anemia)
Results from insufficient B12 intake or poor absorption due to autoimmune conditions or low stomach acid.
Folate Deficiency Anemia
Common in people with poor diets or malabsorption issues.
Hemolytic Anemia
Occurs when red blood cells are destroyed faster than they can be replaced.
Anemia of Chronic Disease
Associated with long-term conditions like autoimmune diseases or infections.
Aplastic Anemia
A rare condition where the bone marrow doesn’t produce enough red blood cells.`
Root Causes of Anemia
🫴🏾 Dietary Deficiencies
Insufficient iron, B12, or folate intake can lead to anemia, especially in restrictive diets.
🫴🏾 Parasitic Infections
Parasites such as hookworms, Giardia, tapeworms, and roundworms can deplete your body of vital nutrients. These parasites feed on their host, robbing them of essential vitamins and minerals, leading to malnutrition and malabsorption.
🫴🏾 Low Stomach Acid (Hypochlorhydria)
Stomach acid is essential for breaking down food and absorbing nutrients like iron and B12. Low stomach acid creates an environment where parasites can thrive and impairs nutrient absorption, leading to anemia.
🫴🏾 Chronic Inflammation
Conditions like autoimmune diseases or infections can disrupt red blood cell production.
🫴🏾 Heavy Menstrual Bleeding
Excessive blood loss during menstruation is a common cause of anemia in women.
The Role of Stomach Acid in Anemia and Parasitic Infections
Low stomach acid (hypochlorhydria) is a key factor in anemia and parasitic infections. Stomach acid kills harmful pathogens and parasites that enter through food or water. When stomach acid is low, these invaders thrive, competing for nutrients and damaging the gut lining, leading to malnutrition and disease.
Reasons for Low Stomach Acid
🌿 Chronic stress
🌿 Poor diet, particularly low protein or processed foods
🌿 Use of acid-reducing medications
🌿 Aging
🌿 Helicobacter pylori infections
How to Prevent Low Stomach Acid
🌿 Eat a nutrient-dense, whole-food diet.
🌿 Manage stress through mindfulness or relaxation techniques.
🌿 Avoid overeating, as it dilutes stomach acid.
🌿 Chew food thoroughly to stimulate digestive enzymes.
🌿 Supplement with digestive bitters or apple cider vinegar if needed.
Diagnosing Anemia: Lab Testing and Functional Ranges
A comprehensive blood panel is essential for understanding anemia. Below are key biomarkers, their standard ranges, and functional ranges:
Primary Biomarkers
Hemoglobin (Hb): Measures oxygen-carrying capacity of red blood cells.
Standard Range: 12–15.5 g/dL (women); 13.5–17.5 g/dL (men)
Functional Range: 13.5–14.5 g/dL (women); 14.5–15.5 g/dL (men)
Ferritin: Indicates iron storage levels in the body.
Standard Range: 12–150 ng/mL
Functional Range: 40–90 ng/mL
Serum Iron: Measures the amount of circulating iron in the blood.
Standard Range: 50–170 µg/dL
Functional Range: 85–130 µg/dL
Vitamin B12: Essential for red blood cell production and nervous system health.
Standard Range: 200–900 pg/mL
Functional Range: 500–1,000 pg/mL
Folate: Critical for DNA synthesis and red blood cell formation.
Standard Range: 2.5–20 ng/mL
Functional Range: 10–15 ng/mL
Secondary Biomarkers for Comprehensive Analysis
White Blood Cells (WBCs): Evaluates immune response and infection.
Standard Range: 4,000–11,000 cells/μL
Functional Range: 5,000–7,000 cells/μL
Red Blood Cells (RBCs): Measures the number of red cells in blood.
Standard Range: 4.2–5.4 million/μL (women); 4.7–6.1 million/μL (men)
Functional Range: 4.4–4.9 million/μL (women); 4.5–5.0 million/μL (men)
Hematocrit (Hct): Indicates the percentage of blood composed of red cells.
Standard Range: 37–47% (women); 42–52% (men)
Functional Range: 37–42% (women); 40–45% (men)
Mean Corpuscular Volume (MCV): Assesses the size of red blood cells.
Standard Range: 80–100 fL
Functional Range: 85–92 fL
Mean Corpuscular Hemoglobin (MCH): Measures the average amount of hemoglobin in a red cell.
Standard Range: 27–31 pg/cell
Functional Range: 28–30 pg/cell
Mean Corpuscular Hemoglobin Concentration (MCHC): Evaluates the concentration of hemoglobin in red cells.
Standard Range: 32–36 g/dL
Functional Range: 33–35 g/dL
Platelets (PLT): Helps assess clotting ability.
Standard Range: 150,000–450,000 cells/μL
Functional Range: 180,000–350,000 cells/μL
Red Cell Distribution Width (RDW): Indicates variability in red cell size, often elevated in anemia.
Standard Range: 11.5–14.5%
Functional Range: 12–13%
Differential White Blood Cell Counts
Neutrophils (%): Indicates bacterial infection or inflammation.
Standard Range: 40–70%
Functional Range: 55–65%
Lymphocytes (%): Reflects viral infections or immune activity.
Standard Range: 20–40%
Functional Range: 25–35%
Monocytes (%): Involves chronic infections or inflammation.
Standard Range: 2–8%
Functional Range: 3–7%
Eosinophils (%): Associated with allergies or parasitic infections.
Standard Range: 1–4%
Functional Range: 1–3%
Basophils (%): Linked to allergic or inflammatory reactions.
Standard Range: 0–1%
Functional Range: <1%
Iron Studies
Iron: Measures circulating iron levels.
Standard Range: 50–170 µg/dL
Functional Range: 85–130 µg/dL
Unsaturated Iron-Binding Capacity (UIBC): Indicates available capacity for iron binding.
Standard Range: 155–355 µg/dL
Functional Range: 150–300 µg/dL
Total Iron-Binding Capacity (TIBC): Evaluates iron transportation.
Standard Range: 250–450 µg/dL
Functional Range: 275–350 µg/dL
Transferrin Saturation: Measures how much transferrin is carrying iron.
Standard Range: 15–50%
Functional Range: 30–40%
Other Relevant Biomarkers
Reticulocyte Count: Indicates bone marrow activity in producing red cells.
Standard Range: 0.5–2.5%
Functional Range: 1–2%
Mean Platelet Volume (MPV): Provides insight into platelet production and activity.
Standard Range: 7.5–11.5 fL
Functional Range: 8–10.5 fL
Additional Functional Tests
🫴🏾 Comprehensive stool analysis to detect parasitic infections.
🫴🏾 Gastric acid secretion tests to evaluate stomach acid levels.
🫴🏾 Micronutrient testing for iron, B12, folate, and other deficiencies.
Why These Biomarkers Matter
Using a combination of these markers helps differentiate between types of anemia, uncover underlying causes, and guide targeted interventions. Functional ranges provide a deeper insight into subclinical issues often overlooked in standard lab tests.
Fun Fact:
Your stomach acid is so strong that it can dissolve metal, yet it’s essential for absorbing delicate nutrients like iron and vitamin B12. Without enough stomach acid, even the healthiest diet can leave you nutrient-deficient!
Comprehensive Anemia Protocol
🌿 Address Nutrient Deficiencies
Supplement with chelated iron, methylated B12, and active folate as needed.
Incorporate iron-rich foods: lentils, spinach, quinoa, and fortified cereals.
🌿 Support Gut Health
Use probiotics and digestive enzymes to enhance absorption.
Treat parasitic infections with herbal remedies like wormwood, black walnut, Cellcore foundational or comprehensive protocol or medical antiparasitics under guidance.
🌿 Optimize Stomach Acid
Consume bone broth, fermented foods, and apple cider vinegar.
Use betaine HCl supplements if recommended.
🌿 Lifestyle Adjustments
Reduce stress with stretching, meditation, or light exercise.
Sleep 7–9 hours nightly to support healing.
Conclusion: Don’t Ignore the Signs
Anemia isn’t just about fatigue; it’s a signal that your body is struggling to get the nutrients it needs. By addressing the root causes—whether nutrient deficiencies, parasitic infections, or low stomach acid—you can restore balance, reclaim energy, and prevent future health complications.
Call to Action: Your Health Deserves Attention
Are you tired of feeling drained, foggy, and unwell? It’s time to uncover the root cause of your symptoms. Don’t settle for a quick
fix—opt for a tailored approach to your health. Book a consultation today and start your journey to vibrant energy and lasting wellness. Your body is ready to heal—are you ready to listen?
Meal: Hearty Lentil and Spinach Stew Over Fluffy Quinoa
A nourishing, vibrant bowl bursting with rich flavors and packed with vital nutrients to uplift your energy and health.
Ingredients
For the Stew:
1 cup lentils: Earthy, tender bites that soak up all the savory goodness.
2 cups fresh spinach: Wilts perfectly into the stew, adding a lush, velvety texture.
1 small sweet potato: Creamy and naturally sweet, balancing the savory spices.
1 juicy tomato, diced: Adds a refreshing, tangy burst of flavor.
1 medium onion and 2 garlic cloves: The aromatic base that makes your kitchen smell divine.
1 teaspoon cumin and 1 teaspoon turmeric: Warming spices that lend an irresistible depth of flavor.
2 cups vegetable broth: Infuses every ingredient with rich, comforting goodness.
1 tablespoon olive oil: Silky and fragrant, bringing it all together.
Salt and pepper: To awaken every ingredient’s natural flavors.
For the Quinoa:
1 cup quinoa: Nutty, light, and the perfect pairing for this hearty stew.
2 cups water and a pinch of salt: Simmered to fluffy perfection.
Instructions
Cook the Quinoa:
Rinse the quinoa, releasing its nutty aroma.
Let it simmer gently, soaking up every drop of water to create light, fluffy grains.
Craft the Stew:
Start by sautéing onions and garlic in olive oil, releasing a heavenly aroma.
Stir in cumin and turmeric for a warm, earthy fragrance that fills the room.
Add the lentils, sweet potato, tomato, and vegetable broth, and let the magic happen as everything simmers to tender perfection.
Fold in vibrant spinach at the end for a pop of color and silky texture.
Assemble Your Bowl:
Scoop the steamy, fragrant quinoa into a bowl.
Ladle over the thick, velvety stew, letting the juices seep into the quinoa.
Garnish with fresh parsley or a squeeze of lemon for a zesty, aromatic finish.
Why You’ll Love It
The Texture: Soft lentils, creamy sweet potato, and tender spinach melt in your mouth, while quinoa adds a delightful nuttiness.
The Flavor: A symphony of warming spices, tangy tomato, and the subtle sweetness of sweet potato creates a truly harmonious dish.
The Nourishment: Every bite feels indulgent but is packed with iron, protein, and vibrant nutrients to energize your body and soul.
Each spoonful is a hug in a bowl—comforting, satisfying, and oh-so-delicious.
Nutritional Benefits:
Iron: Lentils, spinach, and quinoa provide non-heme iron, critical for addressing deficiencies.
Vitamin C: Tomatoes and spinach improve iron absorption.
Protein: Lentils and quinoa offer plant-based complete proteins for energy and recovery.
Antioxidants and Anti-inflammatory Compounds: Turmeric and garlic support overall health and immunity.
This holistic meal aligns with anemia recovery protocols and ensures vibrant health with a balance of essential nutrients.
References:
General Information on Anemia
1. Mayo Clinic. Anemia – Symptoms and Causes.
https://www.mayoclinic.org/diseases-conditions/anemia/symptoms-causes/syc-20351360
2. National Heart, Lung, and Blood Institute (NHLBI). Anemia Overview.
https://www.nhlbi.nih.gov/health/anemia
Parasitic Infections and Their Impact
3. Centers for Disease Control and Prevention (CDC). Parasites – Hookworm.
https://www.cdc.gov/sth/about/hookworm.html?CDC_AAref_Val=https://www.cdc.gov/parasites/hookworm/index.html
4. Journal of Clinical Microbiology. Giardia and Malabsorption Syndromes.
https://jcm.asm.org/
5. WHO. Soil-Transmitted Helminth Infections.
https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
Low Stomach Acid and Its Effects
6. Wright, J. V., & Lenard, L. (2001). Why Stomach Acid is Good for You. McGraw-Hill Education.
7. Functional Medicine University. The Role of Stomach Acid in Digestive Health.
https://www.functionalmedicineuniversity.com
8. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Hypochlorhydria Overview.
https://www.niddk.nih.gov/
Functional and Standard Lab Ranges for Anemia
9. ODX. Clinical Guidelines for Nutrient Deficiencies and Lab Testing.
https://www.optimaldx.com/research-blog/iron-deficiency-without-anemia
10. ODX. Understanding Hemoglobin and Ferritin Lab Results.
https://labtestsonline.org/
11. Cleveland Clinic. Interpreting Vitamin B12 and Folate Levels.
https://my.clevelandclinic.org/
Nutritional and Lifestyle Support for Anemia
12. World Health Organization (WHO). Iron Deficiency Anemia: A Guide for Program Managers.
https://www.who.int/publications/
13. Harvard Health. The Importance of Gut Health in Nutrient Absorption.
https://www.health.harvard.edu
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Vitamin D: The Hormone of Life and Vitality
Vitamin D: The Hormone of Life and Vitality
Imagine a molecule so transformative it modulates over 150 genes, serves as a linchpin for immunity, fortifies your bones, balances hormones, and uplifts mental well-being. Often misunderstood as a mere vitamin, vitamin D functions as a hormone that is indispensable to human health. Its deficiency is a silent epidemic, exacerbating chronic illnesses, immune dysfunction, and hormonal imbalances globally. To fully grasp the depth of its impact and the steps to optimize it, let’s unravel the science and actionable insights behind this extraordinary nutrient.
Understanding Vitamin D Testing: Decoding Your Levels
Optimal health begins with understanding your vitamin D status, which requires precise testing. Here are the two pivotal tests that assess its presence in your body:
1. 25-Hydroxyvitamin D (25(OH)D)
Purpose: This measures the storage form of vitamin D in your bloodstream and is the gold standard for evaluating overall levels.
Conventional Range: 30.00–100.00 ng/mL (74.88–249.60 nmol/L).
Functional Medicine Range: 60.10–90.14 ng/mL (150–225 nmol/L).
2. 1,25-Dihydroxyvitamin D (Calcitriol)
Purpose: This test evaluates the active form of vitamin D. While useful, it may remain stable even during deficiencies, making it a secondary indicator.
Conventional Range: 18.00–72.00 pg/mL (43.20–172.80 pmol/L).
Functional Medicine Range: 35.00–55.00 pg/mL (84.00–132.00 pmol/L).
Key Takeaway: The 25(OH)D test is indispensable for ensuring adequate reserves to support immunity, hormonal harmony, and chronic disease prevention.
Why Vitamin D Matters: Beyond Bone Health
Vitamin D transcends its reputation as merely a bone-supporting nutrient. Its influence permeates every aspect of well-being:
Immune System: Activates T-cells and modulates inflammation, fortifying defenses against infections.
Hormonal Regulation: Balances estrogen and progesterone, aiding in conditions like menstrual irregularities and reducing risks such as fibroids.
Chronic Disease Prevention: Research links adequate vitamin D levels to reduced risks of autoimmune conditions such as, cardiovascular disease, and cancers.
Muscle and Bone Strength: Supports calcium absorption and reduces fracture risk.
Who is at Risk of Deficiency?
Certain demographics face heightened vulnerability to vitamin D insufficiency:
🫴🏾 People with Darker Skin: High melanin levels reduce UVB absorption, limiting natural vitamin D synthesis.
Solution: Regular testing and supplementation tailored to individual needs.
🫴🏾 Northern Latitude Residents: Limited UVB exposure during fall and winter increases risk.
Solution: Supplementation during low sunlight months is essential.
🫴🏾 Older Adults: Age-related decline in skin’s ability to produce vitamin D.
Solution: Increased dietary intake and supplementation.
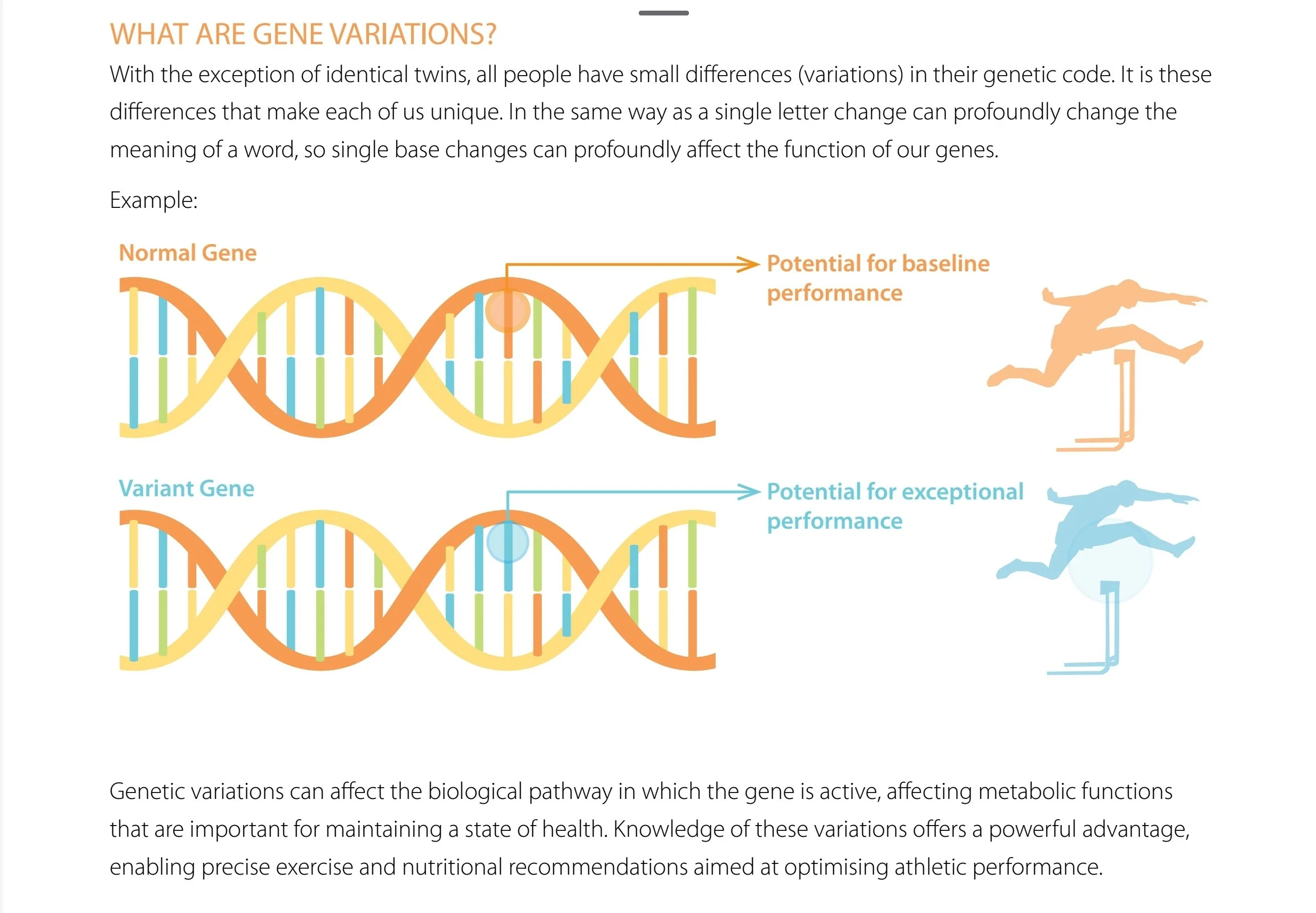
🫴🏾 Genetically Predisposed Individuals: Variants in the GC gene (encoding vitamin D-binding protein) or VDR gene (vitamin D receptor) may impair activation and function.
Recommendation: Genetic testing to personalize supplementation and ensure functional optimization.
🫴🏾 Obese Individuals: Vitamin D is sequestered in fat tissue, making it less bioavailable.
Solution: Higher doses of supplementation under medical guidance.
Harnessing the Sun: Your Natural Vitamin D Source
Sunlight serves as nature’s most potent provider of vitamin D. Here’s how the process works:
🌿 UVB Rays Activate the Skin: Cholesterol in the skin converts to vitamin D3 upon sun exposure.
🌿 Liver and Kidneys Finalize Activation: These organs transform vitamin D3 into calcitriol, the hormone form.
🌿 Systemic Benefits: Calcitriol regulates calcium, enhances immunity, and fosters hormonal equilibrium.
Optimal Exposure: Aim for 10–30 minutes of direct sunlight on bare skin, 2–3 times weekly, between 10 a.m. and 3 p.m. Factors like sunscreen, clothing, and glass windows may necessitate supplementation.
Nourishment Through Whole Food Plant-Based Sources
For those embracing a plant-based lifestyle, dietary options for vitamin D include:
🌿 Mushrooms: Varieties exposed to UV light, such as maitake or portobello, contain vitamin D2.
🌿 Fortified Plant Milks: Almond, soy, or oat milk with added vitamin D.
🌿 Fortified Cereals: Look for organic and non-gmo whole-grain options.
While these can supplement intake, most individuals require additional vitamin D3 from lichen-based supplements for optimal health.
Fun Fact:
Did you know that vitamin D isn't just made in your skin? Mushrooms exposed to sunlight can produce vitamin D2, much like how human skin synthesizes vitamin D3 from UVB rays. This makes them one of the rare plant-based sources of this vital nutrient—perfect for those on a whole food plant-based diet!
Supplementation: Precision for Optimal Health
🫴🏾 Daily Needs: Functional medicine typically recommends 5,000–10,000 IU for adults, far exceeding conventional guidelines.
🫴🏾 Dosing by Age:
Infants: 400–1,000 IU/day.
Children: 1,000–2,000 IU/day.
Adults: 5,000–10,000 IU/day (based on individual requirements).
Note: Always consult with a practitioner to tailor supplementation to your unique needs, especially if you belong to a high-risk group.
Functional Medicine’s Elevated Standards: Optimizing Your Health
Functional medicine prioritizes prevention and vitality, advocating for vitamin D levels within a protective range of 60–90 ng/mL (150–225 nmol/L), surpassing the lower thresholds of conventional guidelines. This approach targets root causes and fosters long-term wellness.
Your Next Step: Reclaiming Your Vitality
Vitamin D is not just a nutrient; it is a cornerstone of health and longevity. By understanding your status, addressing insufficiencies, and leveraging sunlight, food, and targeted supplementation, you can unlock its full potential.
Are you ready to transform your health? Contact us to start with a personalized assessment and take the first step toward vibrant living today.
“Invest in your health, invest in you, because a healthier lifestyle is a luxury you deserve!”
Reference
https://townsendletter.com/vitamin-d-scientific-american-chimes-in-on-vital-as-research-money-vanishes/
https://youtu.be/uAfVC4l5uZ0?si=qXIOdLMK_rservlz
https://youtu.be/y0Wj0kU4-KQ?si=uPN2kUZUez5gLMjc
https://youtu.be/NZI8qJjN2Qw?si=BfOiOnNjpcx9yIyy
https://youtu.be/QAQ7r6jLEww?si=MCTJt9CtFnGYqlE6
https://en.wikipedia.org/wiki/Vitamin_d
https://www.ncbi.nlm.nih.gov/books/NBK278935/
https://www.naturopathy-uk.com/news/news-cnm-blog/blog/2021/06/23/why-is-vitamin-d-important/
https://www.news-medical.net/health/The-Role-of-Vitamin-D-in-Hormonal-Balance.aspx
https://www.evergreen-life.co.uk/health-wellbeing-library/vitamin-d-gateway-to-good-health/
https://www.yourhormones.info/hormones/vitamin-d/
https://adesawell.com/post/optimal-vitamin-d-levels-a-functional-medicine-approach
https://www.pharmacytimes.com/view/vitamin-d-is-the-new-hormone
https://www.vitacost.com/blog/why-is-vitamin-d-important/
https://www.medicalnewstoday.com/articles/161618
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Myth-Busting Facts About a Whole Food Plant-Based Diet
Myth-Busting Facts About a Whole Food Plant-Based Diet
Welcome to a journey toward vibrant health and well-being! As a Seventh-day Adventist Traditional Naturopath, and Functional Diagnostic Nutrition® Practitioner, I'm passionate about helping people discover the incredible power of natural, plant-based nutrition. One of the most compelling examples of the benefits of this lifestyle comes from the Blue Zones—regions of the world where people live the longest, healthiest lives. In these communities, like Okinawa, Japan, and Loma Linda, California, a predominantly plant-based diet is a cornerstone of longevity and vitality.
In this space, we'll explore practical, science-backed insights, and dispel common myths about plant-based nutrition, showing you that you don't need animal products to thrive. Together, we'll uncover the secrets to living your healthiest, happiest life—naturally, and in harmony with the wisdom of the world's longest-living cultures.
Fun Fact:
A fun fact about a whole food plant-based diet is that it can lead to a significant increase in energy levels. Since this diet emphasizes nutrient-dense foods like fruits, vegetables, whole grains, and legumes while avoiding processed foods, it provides your body with high-quality fuel. This can result in feeling more energized throughout the day, with many people reporting better stamina and quicker recovery after exercise. Plus, the diet's high fiber content keeps your digestive system running smoothly, which also contributes to overall well-being and vitality.
Myth #1: You Need Animal Products to Avoid Malnutrition
Fact: A well-planned whole food plant-based diet provides all essential nutrients except for vitamin B12, which can be easily supplemented.
Explanation: One of the most pervasive myths is that a plant-based diet cannot meet all of your nutritional needs, leading to malnutrition. However, this is simply not true. Whole plant foods like fruits, vegetables, legumes, nuts, seeds, and whole grains are packed with vitamins, minerals, fiber, and phytochemicals that support overall health. The only nutrient that needs supplementation is vitamin B12, which is not produced by plants but is essential for nerve function and red blood cell formation.
Evidence: The Academy of Nutrition and Dietetics states that appropriately planned vegetarian and vegan diets are nutritionally adequate and may provide health benefits for the prevention and treatment of certain diseases . The Adventist Health Study-2, which analyzed the health outcomes of over 96,000 Seventh-day Adventists, found that those who followed a vegetarian diet, especially a vegan diet, had lower rates of heart disease, diabetes, and certain cancers compared to those who consumed meat.
Myth #2: Animal Products Are Necessary for Gut Health
Fact: A plant-based diet, rich in fiber, is superior for gut health and promotes a diverse and balanced gut microbiome.
Explanation: The gut microbiome is made up of trillions of bacteria and other microorganisms that play a crucial role in digestion, immune function, and even mental health. Fiber, found abundantly in plant foods, is a key nutrient for feeding the beneficial bacteria in your gut. These bacteria ferment fiber into short-chain fatty acids (SCFAs), which support gut health and reduce inflammation.
Evidence: Studies show that a diet high in fiber from plant-based sources is associated with a more diverse microbiome, which is linked to better overall health. Conversely, diets high in animal products and low in fiber can disrupt the balance of gut bacteria, leading to dysbiosis and increased risk of conditions like inflammatory bowel disease (IBD).
Myth #3: Animal Products Are Necessary for a Healthy Sex Steroid Hormone Cascade
Fact: A whole food plant-based diet supports a healthy hormone balance, including the sex steroid hormone cascade, without the need for animal products.
Explanation: The sex steroid hormone cascade involves hormones like estrogen, progesterone, and testosterone, which are crucial for reproductive health, sexual function, and overall vitality. There’s a common misconception that animal products are essential for maintaining these hormones at optimal levels. However, consuming a diet rich in whole plant foods can provide the necessary nutrients to support healthy hormone production and balance.
Evidence: Plant-based diets are rich in phytonutrients, such as lignans found in flaxseeds, which have been shown to support healthy estrogen levels by modulating estrogen metabolism. Additionally, a diet high in fruits, vegetables, and whole grains provides an abundance of antioxidants and anti-inflammatory compounds that protect the body from oxidative stress, which can disrupt hormone production.
Conversely, diets high in animal fats have been associated with increased levels of sex hormone-binding globulin (SHBG), a protein that binds to sex hormones and reduces their bioavailability, potentially leading to imbalances. A study published in *The American Journal of Clinical Nutrition* found that individuals consuming plant-based diets had lower levels of SHBG and more balanced levels of free sex hormones compared to those consuming high amounts of animal products.
Moreover, the consumption of dairy products, which contain natural bovine hormones, has been linked to disruptions in the human endocrine system. This can potentially lead to conditions like hormonal acne, menstrual irregularities, and an increased risk of hormone-related cancers.
By choosing a whole food plant-based diet, you can support a healthy sex steroid hormone cascade naturally, without the need for animal products.
Myth #4: Plant-Based Diets Cause Brain Fog and Mood Swings
Fact: A well-balanced plant-based diet can improve brain function and stabilize mood.
Explanation: Brain fog and mood swings are often mistakenly attributed to plant-based diets, but the truth is that these issues are more commonly associated with diets high in processed foods, sugar, and unhealthy fats. Plant-based diets, which are rich in antioxidants, healthy fats, and complex carbohydrates, can actually enhance brain function and mood.
Evidence: Omega-3 fatty acids, found in flaxseeds, chia seeds, and walnuts, are essential for brain health and can be adequately obtained from plant sources. Additionally, the high levels of antioxidants in fruits and vegetables help reduce oxidative stress and inflammation in the brain, which can improve cognitive function and mood . Studies have shown that individuals who follow a plant-based diet have lower levels of anxiety and depression, likely due to the diet’s anti-inflammatory properties.
Myth #5: Plant-Based Diets Lead to Mold Toxicity
Fact: Mold toxicity is more commonly associated with certain foods like grains, nuts, and coffee, but a whole food plant-based diet can actually help reduce the risk.
Explanation: While it’s true that certain plant-based foods, such as grains and nuts, can be contaminated with molds that produce mycotoxins, this issue is not exclusive to plant-based diets. Proper storage and preparation methods can significantly reduce the risk. Moreover, the antioxidants and phytonutrients found in a whole food plant-based diet can help detoxify the body and support the liver in processing and eliminating toxins.
Evidence: Studies indicate that a diet rich in vegetables and fruits can enhance the body’s natural detoxification processes. For example, cruciferous vegetables like broccoli and Brussels sprouts contain compounds that support liver function and help protect against toxin-related damage.
Myth #6: The Blue Zones’ Longevity Is Due to Animal Products
Fact: The diets of the Blue Zones—regions with the highest concentration of centenarians—are predominantly plant-based, with animal products playing a minimal role.
Explanation: The Blue Zones, including Okinawa (Japan), Sardinia (Italy), Ikaria (Greece), Nicoya (Costa Rica), and Loma Linda (California), share common dietary patterns that are mostly plant-based. These communities consume diets rich in legumes, whole grains, vegetables, and nuts, with meat and dairy products used sparingly, often only a few times a month.
Evidence: In Loma Linda, California, home to a large population of Seventh-day Adventists, many people follow a vegetarian or vegan diet. Research shows that Adventists who adhere to a plant-based diet live significantly longer than the general population, with lower rates of chronic diseases such as heart disease, cancer, and diabetes . Similarly, in Okinawa, the traditional diet consists of sweet potatoes, soy products, and green leafy vegetables, with very little meat, leading to one of the highest life expectancies in the world.
Did you know
It is a mistake to suppose that muscular strength depends on the use of animal food. The needs of the system can be better supplied, and more vigorous health can be enjoyed, without its use. The grains, with fruits, nuts, and vegetables, contain all the nutritive properties necessary to make good blood. These elements are not so well or so fully supplied by a flesh diet. Had the use of flesh been essential to health and strength, animal food would have been included in the diet appointed man in the beginning.
When the use of flesh food is discontinued, there is often a sense of weakness, a lack of vigor. Many urge this as evidence that flesh food is essential; but it is because foods of this class are stimulating, because they fever the blood and excite the nerves, that they are so missed. Some will find it as difficult to leave off flesh eating as it is for the drunkard to give up his dram; but they will be the better for the change. -EGW
Blue Zones: Living Proof of Plant-Based Benefits
Blue Zones are regions where people live significantly longer and healthier lives. These areas include Okinawa (Japan), Ikaria (Greece), Sardinia (Italy), Nicoya Peninsula (Costa Rica), and Loma Linda (California). A common thread among these regions is a diet that is predominantly plant-based.
Key Dietary Patterns in Blue Zones
🌿 High Consumption of Beans and Legumes: Beans are a staple in Blue Zones, providing a rich source of protein, fiber, and essential nutrients. For example, the traditional diet in Okinawa includes soybeans, while the Nicoya Peninsula diet features black beans.
🌿 Minimal Meat Consumption: While some Blue Zones include small amounts of meat, it is consumed sparingly. In Loma Linda, home to a large population of Seventh-day Adventists, many individuals follow a vegetarian or vegan diet, contributing to their longevity and lower rates of chronic diseases[1][2].
🌿 Whole Foods Over Processed Foods: Blue Zone diets emphasize whole, minimally processed foods. This includes a variety of vegetables, fruits, nuts, seeds, and whole grains. For example, Ikaria's diet includes a wide range of wild greens and herbs, which are rich in antioxidants and polyphenols[4].
Health Outcomes in Blue Zones
Research indicates that the dietary habits in Blue Zones contribute to remarkable health outcomes:
🫴🏾 Increased Lifespan: People in Blue Zones often live to be over 100 years old. For instance, Seventh-day Adventists in Loma Linda have a life expectancy that is 10 years longer than the average American[1][4].
🫴🏾 Lower Rates of Chronic Diseases: Plant-based diets in Blue Zones are associated with lower rates of heart disease, diabetes, and certain cancers. This is attributed to the high intake of fiber, antioxidants, and anti-inflammatory compounds found in plant foods[4].
Conclusion: Embracing the Power of a Whole Food Plant-Based Diet
The myths surrounding plant-based diets are persistent, but science and the lived experiences of long-lived populations show that you don’t need animal products to thrive. A whole food plant-based diet is rich in all the essential nutrients your body needs, supports gut health, promotes hormonal balance, and protects against chronic diseases. By focusing on a variety of whole, unprocessed plant foods, you can enjoy vibrant health and potentially extend your lifespan, much like the centenarians in the Blue Zones.
If you’re considering transitioning to a whole food plant-based diet, rest assured that you’re making a choice that is not only good for your body but also for the planet. With the right information and support, you can easily adopt this way of eating and reap the many benefits it offers.
When flesh food is discarded, its place should be supplied with a variety of grains, nuts, vegetables, and fruits that will be both nourishing and appetizing. This is especially necessary in the case of those who are weak or who are taxed with continuous labor. In some countries where poverty abounds, flesh is the cheapest food. Under these circumstances the change will be made with greater difficulty; but it can be effected. We should, however, consider the situation of the people and the power of lifelong habit, and should be careful not to urge even right ideas unduly. None should be urged to make the change abruptly. The place of meat should be supplied with wholesome foods that are inexpensive. In this matter very much depends on the cook. With care and skill, dishes may be prepared that will be both nutritious and appetizing, and will, to a great degree, take the place of flesh food. -EGW
High Protein Butter Bean Tofu Stew
This creamy, flavorful dish is ready in just 30 minutes! Packed with 32g of protein and 10g of fiber per serving, this butter bean and tofu stew is both nourishing and satisfying. Plus, it’s made with simple, easy-to-find ingredients for a hassle-free meal.
Prep Time
10 minutes
Cook Time
20 minutes
Ingredients
280g firm tofu broken up into chunks
1 tbsp cornflour or arrowroot flour
1 tbsp Gram masala seasoning
2 tbsp Avocado oil divided
1/2 onion chopped
3 garlic cloves minced or more to taste
1 can butter beans drained and rinsed
200g baby plum tomatoes slices in half or canned tomatoes
1 tsp turmeric powder
1/2 tsp chilli powder
100 ml oat cream or coconut milk
Juice of 1 lemon
Salt & cayenne pepper to taste
To serve
Fresh coriander
Chilli flakes
Rice or quinoa for extra protein
For the salad
2 tomatoes
1/2 cucumber
1 tbsp chopped onions
1/2 tbsp lemon juice
1/2 tbsp Avocado oil
Salt & cayenne pepper to taste
Instructions
Break up the tofu into chunks and place in a bowl. Add 1 tbsp cornflour, tamari sauce and gram masala, oil and toss to coat.
Place on a baking tray lined with parchment paper and bake in a preheated oven at 200°C (400°F) for 20 to 25 minutes.
Heat 1 tablespoon of oil in a pan and sauté the onions until golden and fragrant, about 5 minutes. Toss in the juicy tomatoes and garlic, letting them soften and release their rich, savory juices.
Stir in the butter beans, zesty lemon juice, velvety cream, and a medley of aromatic spices. Season generously with salt and pepper, and let the flavors meld together, simmering for 5–10 minutes. The result? A creamy, flavor-packed dish bursting with irresistible warmth and comfort.
Gently fold in the tofu, letting it soak up the rich, aromatic spices. Cook until the tofu is warm and infused with flavor, and every bite bursts with the perfect blend of seasonings.
Prepare the salad by mixing all the ingredients in a bowl.
Garnish with fresh coriander, a sprinkle of chilli flakes, rice and the homemade salad.
Health Benefits of Ingredients
Tofu 🥢: High in protein for muscles & rich in calcium for strong bones.
Butter Beans 🫘: Packed with fiber for digestion & potassium for heart health.
Avocado Oil 🥑: Heart-healthy fats & skin-loving vitamin E.
Garlic 🧄: Boosts immunity & lowers inflammation.
Tomatoes 🍅: Loaded with antioxidants for glowing skin.
Turmeric ✨: Anti-inflammatory powerhouse for joint health.
Chilli 🌶️: Speeds up metabolism & adds a spicy kick.
Lemon 🍋: Detoxifies & boosts vitamin C.
Coriander 🌿: Aids digestion & detox support.
Rice/Quinoa 🍚: Energy boost & complete plant protein.
Simple, healthy, and delicious! 🌟
Citations:
[1] https://www.healthline.com/nutrition/seventh-day-adventist-diet
[2] https://zoe.com/learn/podcast-longevity-according-to-blue-zones
[4] https://www.bluezones.com/2020/07/blue-zones-diet-food-secrets-of-the-worlds-longest-lived-people/
[5] https://www.zoeharcombe.com/2011/08/the-vegetarian-myth-lierre-keith/
[7] https://www.reddit.com/r/nutrition/comments/18zlku4/you_are_what_you_eat_netflix/
Citations for the studies mentioned:
Melina, V., Craig, W., & Levin, S. (2016). "Position of the Academy of Nutrition and Dietetics: Vegetarian Diets." Journal of the Academy of Nutrition and Dietetics, 116(12), 1970-1980. [https://www.sciencedirect.com/science/article/abs/pii/S2212267216311923]
Fraser, G. E. (2009). "Vegetarian diets: what do we know of their effects on common chronic diseases?" The American Journal of Clinical Nutrition, 89(5), 1607S-1612S. [https://academic.oup.com/ajcn/article/89/5/1607S/4596792]
Hills, R. D., et al. (2019). "Gut Microbiome: Profound Implications for Diet and Disease." Nutrients, 11(7), 1613. [https://www.mdpi.com/2072-6643/11/7/1613]
Zeng, Y., et al. (2016). "Effect of vegetarian diet on gut microbiota: an updated review." Frontiers in Nutrition, 3, 31. [https://www.frontiersin.org/articles/10.3389/fnut.2016.00031/full]
Jacka, F. N., et al. (2017). "A randomized controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial)." BMC Medicine, 15, 23. [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-017-0791-y]
Recipe inspired by:
https://nadiashealthykitchen.com/butter-bean-tofu-stew/
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
"Women's Hormonal Health: Navigating Menstrual Cycles and Wellness"
Women's Hormonal Health: Navigating Menstrual Cycles and Wellness
Women's hormonal health plays a vital role in overall wellness, influencing menstrual cycles, mood, energy levels, and reproductive health. As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I take a holistic and investigative approach to identifying and addressing the root causes of hormonal imbalances. Combining this with a whole food plant-based (WFPB) diet offers a powerful and natural strategy to optimize hormonal health. This article explores how a WFPB diet, personalized assessments, and integrative lifestyle tools such as cycle trackers can support women in navigating their menstrual cycles and achieving optimal wellness.
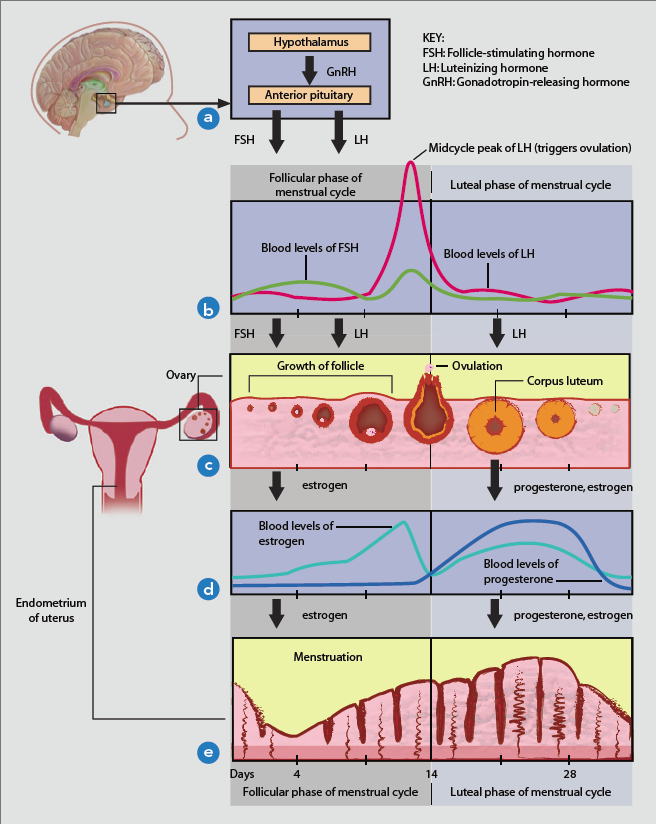
Understanding the Menstrual Cycle
The female cycle begins with the follicular phase. During this phase, the brain releases FSH (Follicle-stimulating hormone) which stimulates the growth of ovarian follicles. As these follicles mature, they produce estrogen, leading to increased estrogen levels in the body. At this stage, estrogen levels should be higher than progesterone levels. As estrogen secretion continues to rise, FSH levels start to decline, and LH (Luteinizing hormone) is released. This culminates in a sharp rise in estrogen, a surge of LH, and a small burst of FSH, resulting in the release of the mature egg. This marks the transition to the luteal phase, where the corpus luteum forms around the egg and releases small amounts of estrogen and predominantly progesterone.
The menstrual cycle is regulated by a complex interplay of hormones, mainly estrogen and progesterone. It typically lasts around 28 days but can range from 21 to 35 days. The cycle is divided into four phases:
Understanding the menstrual cycle phases
1. Menstrual Phase (Days 1-5): The uterine lining is shed, resulting in menstrual bleeding.
2. Follicular Phase (Days 1-13): This phase overlaps with menstruation and involves the maturation of ovarian follicles and a rise in estrogen, thickening the uterine lining.
3. Ovulation (Day 14): A surge in Luteinizing Hormone (LH) triggers the release of an egg from the dominant follicle.
4. Luteal Phase (Days 15-28): The ruptured follicle forms the corpus luteum, which produces progesterone to prepare the uterine lining for potential pregnancy. If fertilization does not occur, progesterone levels fall, leading to menstruation.
Using Cycle Trackers to Understand Hormonal Health
Incorporating cycle tracking tools is a practical way to monitor and understand menstrual health. Trackers such as Natural Cycles° and the Oura Ring can help identify patterns, hormonal shifts, and potential imbalances.
Benefits of Cycle Tracking
🫴🏾 Identifying Patterns and Imbalances: Observe irregularities such as delayed ovulation or inconsistent cycles, which may indicate hormonal imbalances.
🫴🏾 Optimizing Lifestyle Choices: Adjust nutrition, exercise, and stress management strategies to align with different phases of the cycle.
🫴🏾 Enhanced Fertility Awareness: Provide a natural, hormone-free method to determine fertile windows for those seeking to conceive or avoid pregnancy.
🫴🏾 Improved Symptom Management: Highlight correlations between hormonal fluctuations and lifestyle factors, offering actionable insights for symptom relief.
Overview of Key Trackers
🫴🏾 Purpose: A digital fertility and birth control tracker.
🫴🏾 Features: Uses basal body temperature (BBT) to predict ovulation and fertile days.
🫴🏾 Benefits: Hormone-free, FDA-cleared, and ideal for natural contraception or detailed cycle monitoring.
Oura Ring:
🫴🏾 Purpose: A wearable health tracker monitoring physiological markers like body temperature, heart rate variability, and sleep.
🫴🏾 Features: Tracks temperature trends to indicate cycle phases, predict ovulation, and identify disruptions.
🫴🏾 Benefits: Combines cycle tracking with broader wellness insights, helping users understand the impact of sleep, stress, and activity on hormonal health.
By using these tools, women can develop a deeper understanding of their bodies, empowering them to make informed decisions to support overall well-being. To help you get started, download our free Period Preparation Self-Care Checklist and take the first step toward a healthier cycle.
A Holistic Approach to Women's Hormonal Health: Balancing Menstrual Cycles with Naturopathy and Functional Diagnostic Nutrition® and a Whole Food Plant-Based Diet
Traditional Naturopaths and FDN practitioners use a holistic and investigative approach to hormonal health, focusing on identifying and addressing root causes of imbalances. Combining this approach with a WFPB diet enhances the body's ability to maintain hormonal balance naturally.
Comprehensive Assessment in FDN
Functional Diagnostic Nutrition® practitioners start with a thorough health assessment, combining medical history, lifestyle, and lab tests. This comprehensive evaluation helps tailor a specific approach for each woman, focusing on balancing hormonal health naturally. For menstrual health and overall wellness, the following functional labs play an integral role:
Key Functional Lab Tests
DUTCH Test (Dried Urine Test for Comprehensive Hormones): This test evaluates adrenal and sex hormones, including estrogen, progesterone, testosterone, cortisol, and melatonin. It is especially important for understanding the balance of estrogens (E1, E2, E3) and their metabolites, which influence menstrual cycles, PMS, fertility, and perimenopausal symptoms.
DNALife Estrogen and Health Test: A genetic test identifying variations in estrogen metabolism and detoxification pathways to address hormonal imbalances like estrogen dominance and PMS, guiding personalized wellness strategies.
Comprehensive Thyroid Panel: Hormonal imbalances can stem from thyroid dysfunction. Testing for TSH (Thyroid-Stimulating Hormone), Free T3 (Triiodothyronine, Free T4 (Thyroxine), reverse T3 (rT3), and thyroid antibodies [TPO (Thyroid Peroxidase Antibodies) and TgAb (Thyroglobulin Antibodies)] helps assess thyroid health, which impacts metabolism, menstrual regularity, and energy levels.
GI-MAP (Gastrointestinal Microbial Assay Plus): The GI-MAP stool test assesses gut health, which is crucial for hormone metabolism and detoxification. Gut dysbiosis, infections, and inflammation can affect estrogen balance and lead to symptoms like bloating, acne, and heavy periods. Proper gut function supports estrogen clearance, reducing estrogen dominance.
Micronutrient Testing: This test evaluates vitamin and mineral levels essential for hormone production and regulation. Deficiencies in magnesium, zinc, B vitamins (especially B6, B12, and folate), and vitamin D can lead to PMS, menstrual irregularities, and fatigue.
Comprehensive Metabolic Panel (CMP): This test provides a general overview of organ function, glucose regulation, and electrolyte balance, all of which are critical for maintaining hormonal homeostasis.
The Traditional Naturopathic and Functional Diagnostic Nutrition® Approach with a WFPB Diet
Benefits of a Whole Food Plant-Based Diet
A Whole Food Plant-Based (WFPB) diet can offer numerous benefits for women's hormonal health, particularly in managing the menstrual cycle. This approach emphasizes unprocessed, plant-based foods, which are naturally rich in essential nutrients that support hormone regulation. Some key benefits include:
Improved Estrogen Metabolism:
High-fiber diets help in the elimination of excess estrogen through the digestive system, reducing the risk of estrogen dominance, which is linked to PMS, heavy menstrual bleeding, and even conditions like fibroids or endometriosis.
Anti-inflammatory Properties:
Plant-based diets, rich in antioxidants, phytonutrients, and omega-3 fatty acids (found in flaxseeds, chia seeds, and walnuts), can reduce systemic inflammation, which is often associated with painful periods and hormonal imbalances.
Blood Sugar Regulation:
Whole grains, legumes, and vegetables provide complex carbohydrates that help stabilize blood sugar levels. Balanced blood sugar is crucial for maintaining steady energy levels throughout the menstrual cycle and preventing mood swings or irritability.
Support for Mitochondrial Function:
Mitochondrial health is critical for energy production and hormone synthesis. A nutrient-dense, plant-based diet can provide the necessary vitamins and minerals (e.g., B vitamins, magnesium, and iron) needed to support healthy mitochondrial function, thus reducing fatigue and improving overall energy, especially during menstruation.
Fun Fact
A fun fact about women on a whole food plant-based diet is that studies have shown it can have significant health benefits, including reducing the risk of heart disease, improving blood sugar control, and promoting healthy weight management. Plant-based diets are rich in fiber, vitamins, and antioxidants, which can support overall well-being and longevity.
Personalized Nutrition and Dietary Strategies
In Traditional Naturopathy and Functional Diagnostic Nutrition® (FDN), personalizing nutrition is key to addressing individual hormonal needs. Women have varying hormonal landscapes depending on factors like age, stress, and overall health, so the WFPB diet must be tailored to these factors:
🌿 Cycle-Specific Nutrition:
Nutritional needs vary throughout the menstrual cycle. For example, during the follicular phase, focus on foods rich in phytoestrogens (e.g., flaxseeds, soy) that can support healthy estrogen levels. In the luteal phase, which can often be characterized by PMS symptoms, increasing magnesium-rich foods (like leafy greens, seeds, and nuts) can help ease cramps and mood disturbances.
🌿 Addressing Nutrient Deficiencies:
Women may be more prone to deficiencies in iron, calcium, and vitamin D due to menstrual blood loss. Incorporating plant-based sources of these nutrients, such as lentils, tofu, and fortified plant milks, is essential for maintaining bone health and preventing fatigue. Supplementing with B12 and omega-3s may also be necessary for those on strict WFPB diets.
🌿 Gut Health Focus:
A healthy gut microbiome is linked to balanced hormone production and metabolism. Fermented foods like sauerkraut, kimchi, and miso, along with prebiotic-rich foods like garlic, onions, and asparagus, can enhance gut health and in turn support hormone balance.
🌿 Supporting Detoxification:
Cruciferous vegetables (e.g., broccoli, kale, cauliflower) contain compounds that support liver detoxification pathways, helping to metabolize and excrete excess hormones. Detoxification is a crucial part of managing hormonal imbalances related to PMS or other menstrual disorders.
Lifestyle Modifications
In addition to dietary changes, lifestyle interventions play a significant role in managing hormonal health. While stretching is often recommended, there are other impactful strategies that can complement a WFPB diet:
Stress Management through Mindfulness and Meditation:
Chronic stress can lead to dysregulated cortisol levels, which interfere with reproductive hormones. Implementing mindfulness techniques, meditation, or even deep-breathing exercises can help reduce stress and cortisol levels, promoting hormonal balance.
Sleep Optimization:
Poor sleep affects hormone production, including melatonin and cortisol, and can worsen PMS symptoms. Ensuring adequate, quality sleep (8-10 hours per night) by establishing a regular sleep routine, reducing blue light exposure before bed, and creating a calming pre-sleep ritual can aid in hormonal balance.
Strength and Resistance Training:
Physical exercise, particularly resistance training, can help regulate insulin levels, support metabolic health, and reduce PMS symptoms. Weight-bearing exercises also improve bone density, which is crucial for women, especially as they age and face changes in estrogen levels that impact bone health.
Environmental Toxin Reduction:
Exposure to endocrine-disrupting chemicals (EDCs) in plastics, cosmetics, and cleaning products can interfere with hormone function. Reducing exposure by choosing natural, non-toxic personal care products and avoiding plastic containers for food and drink storage can help support hormonal balance.
Key Supplements for Women’s Hormonal Health
Based on common patterns seen in women’s hormonal health and whole food plant-based diets, targeted supplementation may include:
🌿 Magnesium (Bioptimizer Magnesium Breakthrough)
Magnesium is crucial for the enzymatic processes that support hormonal balance, reduce cramping, and alleviate PMS symptoms. It also plays a key role in stress reduction, which can help manage cortisol levels.
🌿 Omega-3 Fatty Acids (Algae-based DHA/EPA)
For those on plant-based diets, algae-based omega-3 supplements can support hormonal health, reduce inflammation, and promote balanced prostaglandin production, essential for easing menstrual discomfort.
🌿 B-Complex Vitamins (Designs for Health)
B vitamins, particularly B6, support progesterone production and balance estrogen metabolism. B12 and folate are essential for cellular energy and methylation, often needed in plant-based diets since they can be deficient.
🌿 Adaptogens (Ashwagandha from Cellcore)
Adaptogenic herbs like ashwagandha help balance the adrenal glands, supporting cortisol regulation. This, in turn, helps manage menstrual irregularities, improve energy, and reduce stress-related hormonal imbalances.
🌿 Vitamin D3 with K2 (Designs for Health)
Vitamin D is critical for modulating the immune system, supporting progesterone production, and enhancing mood regulation. Since plant-based diets can sometimes lack adequate vitamin D, supplementation is key, particularly when lab tests indicate a deficiency.
🌿 Zinc (Zinc Picolinate by Thorne)
Zinc is vital for ovulation and supports the luteal phase of the menstrual cycle. It is also necessary for immune function and healthy skin, often needing to be supplemented in a plant-based diet.
🌿 Evening Primrose Oil or Borage Oil (Plant-based options)
These oils are rich in gamma-linolenic acid (GLA), an omega-6 fatty acid that supports estrogen balance and may reduce symptoms of PMS, like breast tenderness and bloating.
Supporting Detox Pathways
Estrogen dominance is a common issue in hormonal imbalance, where the body has too much estrogen relative to progesterone. To support estrogen detoxification:
🌿 DIM (Diindolylmethane) from Thorne or Integrative Therapeutics supports the liver’s ability to metabolize and excrete excess estrogen.
🌿 Liver Support (Milk Thistle, Dandelion Root): from Cellcore or Gaia Herbs offers liver-supporting herbs to enhance estrogen detoxification.
Where to buy:
International- KXCTGG
Case Study: Holistic Approach to PCOS with a WFPB Diet
Consider Anna, a 28-year-old woman diagnosed with Polycystic Ovary Syndrome (PCOS). She experiences irregular periods, weight gain, and acne. An FDN approach with a WFPB diet would involve:
Comprehensive Testing: Assessing insulin levels, androgens, thyroid function, and inflammatory markers.
Personalized Nutrition: Implementing a low-glycemic, anti-inflammatory WFPB diet to manage insulin resistance and reduce inflammation.
Targeted Supplements: Using inositol to improve insulin sensitivity, and omega-3 fatty acids to reduce inflammation.
Lifestyle Modifications: Incorporating stress reduction techniques, regular moderate exercise, and improving sleep hygiene.
Ongoing Support: Regular follow-ups to adjust the plan based on symptom improvements and test results.
Conclusion
A whole food plant-based diet, integrated with the principles of Traditional Naturopath and Functional Diagnostic Nutrition®, offers a personalized and holistic approach to women's hormonal health. By focusing on comprehensive assessments, individualized nutrition, targeted supplementation, and lifestyle modifications, FDN practitioners help women navigate their menstrual cycles and achieve optimal hormonal balance. Whether dealing with common menstrual issues or more complex conditions like PCOS and endometriosis, this combined approach provides a natural and effective pathway to lasting wellness. If you want to hire a Functional Diagnostic Nutrition® Practitioner to help you with your menstrual cycle do so today! Take advantage of our Complimentary Discovery Call 🤙🏾 today!
Citations:
1. Benefits of a Whole Food Plant-Based Diet:
Whole food plant-based diets are rich in fiber, phytonutrients, and antioxidants, which help balance hormones, reduce inflammation, and improve metabolic health【42】【43】【44】.
They also support gut health and estrogen detoxification through fiber-rich foods like leafy greens, flaxseeds, and whole grains【42】【44】.
Sources:
Purely Planted: 7 Plant-Based Foods for Hormonal Balance
Cleveland Clinic: What You Should Know About Plant-Based Diets
https://health.clevelandclinic.org
Plant-Based Mavens: Plant-Based Diet Benefits for Women
2. Personalized Lab Testing (DNALife Estrogen and Health Test):
This genetic test evaluates pathways for estrogen metabolism and detoxification, helping to address hormonal imbalances such as estrogen dominance. It provides actionable insights for tailoring dietary and lifestyle interventions【42】【44】.
3. Using Cycle Trackers:
Tools like Natural Cycles and Oura Ring provide personalized insights into menstrual patterns and hormonal shifts, empowering women to optimize lifestyle strategies. These tools also assist in fertility tracking and symptom management【42】【43】.
Sources:
Purely Planted: 7 Plant-Based Foods for Hormonal Balance
Cleveland Clinic: What You Should Know About Plant-Based Diets
https://health.clevelandclinic.org
4. Key Supplements and Nutritional Focus:
The inclusion of nutrients like magnesium, omega-3s, and B-complex vitamins supports hormonal balance and addresses deficiencies common in plant-based diets. Evidence suggests that omega-3s reduce inflammation, while magnesium alleviates PMS symptoms【43】【44】.
Sources:
Cleveland Clinic: What You Should Know About Plant-Based Diets
https://health.clevelandclinic.org
Plant-Based Mavens: Plant-Based Diet Benefits for Women
DISCLAIMER. The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Understanding Metabolic Chaos®: The Root Cause of Your Health Challenges
Understanding Metabolic Chaos®: The Root Cause of Your Health Challenges
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I often see clients who are frustrated and overwhelmed after months and sometimes years of trying to resolve their health issues. They’ve seen multiple specialists, tried various treatments, and still aren’t feeling better. This cycle of trial and error can be exhausting, and it’s a sign that something deeper may be at play. Introducing Metabolic Chaos®—a holistic approach to uncovering the root causes of seemingly unrelated health symptoms and providing a clear path to healing.
What is Metabolic Chaos®?
Metabolic Chaos® refers to the hidden dysfunctions occurring in the body’s interconnected systems—hormonal regulation, immune function, digestion, detoxification, energy production, and oxidative stress (H.I.D.D.E.N.O). Our bodies are designed to function as a cohesive whole—when one system is out of balance, it often affects others. Chronic fatigue, brain fog, digestive issues, hormonal imbalances—these aren’t isolated problems. They are all signs of a deeper imbalance, where multiple bodily systems are struggling to communicate and function optimally.
At the heart of Metabolic Chaos® is the idea that the body works as a dynamic network. These H.I.D.D.E.N.O systems are deeply interconnected; when one area is off, it causes a ripple effect that disrupts others systems. This chaos can create a confusing web of symptoms, which is why it’s crucial to look at the bigger picture rather than addressing symptoms in isolation.
The H.i.d.d.e.n.o Drivers of Metabolic Chaos®
Many common health complaints stem from hidden factors within the body. By understanding how these hidden contributors interact, we can begin to identify the root causes of your health challenges.
🍃 Hormonal Imbalances: Hormones are chemical messengers that regulate almost every function in your body, from metabolism to mood. When your hormones are out of balance, you may experience fatigue, weight gain, low libido, or brain fog. These imbalances are often linked to stress, poor diet, or other underlying issues like oxidative stress, which impacts how your cells and tissues function.
🍃 The Immune System: Chronic inflammation, allergies, or frequent infections could be signs that your immune system is in overdrive, which impacts everything from gut health to hormone balance. Dysbiosis (an imbalance in gut bacteria) and poor mucosal integrity can disrupt your immune system, leaving you susceptible to further issues like digestive problems, skin conditions, or autoimmune responses.
🍃 Digestive System: When digestion is compromised, you may experience symptoms like bloating, gas, or indigestion. These issues are often linked to deeper dysfunctions, such as an imbalance in your gut microbiome, stress, or liver congestion. Over time, poor digestion affects your nutrient absorption, immune function, and even your mood.
🍃 Detoxification Pathways: Your body has a natural detoxification system, but if it’s overloaded by environmental toxins, poor diet, or stress, your liver and kidneys can’t keep up. This results in fatigue, skin issues, headaches, or stubborn weight gain. When detox pathways are clogged, other systems like digestion and hormone regulation also begin to suffer.
🍃 Energy Production: When your body struggles to produce energy efficiently, it’s often due to imbalances in cellular metabolism. Symptoms like fatigue, brain fog, and poor concentration can all point to issues with energy production. These energy deficits can also affect how well your body heals, fights off illness, or maintains hormonal balance.
🍃 Nervous System Dysregulation: The autonomic nervous system, which regulates your body’s stress response, can become overburdened by chronic stress, poor sleep, or emotional imbalances. This leads to symptoms like anxiety, poor mood regulation, and even digestive or immune problems. Over time, chronic nervous system dysregulation can become a root cause of further metabolic chaos.
🍃 Oxidative Stress: This occurs when there’s an imbalance between free radicals and antioxidants in your body. Oxidative stress damages cells, leading to aging, chronic inflammation, and even disease. If you’re exposed to environmental toxins, processed foods, or chronic stress, oxidative stress can lead to energy depletion, poor immune function, and accelerated aging.
Identifying Metabolic Chaos®: The First Step Towards Healing
Through my practice, I use specialized functional lab tests, Nutrigenetics tests, and assessments to uncover these H.I.D.D.E.N.O drivers of Metabolic Chaos®. These tests give me insight into how your body’s systems are functioning and where imbalances may lie. For example, hormone tests reveal adrenal and cortisol dysfunction, gut health tests identify dysbiosis or intestinal permeability “leaky gut”, and oxidative stress markers highlight cellular damage. By identifying where the weak links are, we can create a tailored plan to restore balance across your body’s systems.
Restoring Balance: A Holistic Healing Plan
Once I have identified the root causes of your health challenges, I will put together a comprehensive protocol. This typically includes:
Dietary Adjustments: Nutrient-dense, anti-inflammatory foods that support gut health, balance blood sugar, and reduce oxidative stress.
Targeted Supplements: Adaptogenic herbs to support stress response, probiotics for gut health, or antioxidants to combat oxidative stress.
Lifestyle Changes: Stress management techniques like meditation, improved sleep hygiene, exercise such as strength training, and gentle movement practices like stretching or walking to support nervous system regulation.
Detox Support: Nutritional and lifestyle changes that enhance liver function and reduce your exposure to environmental toxins.
Fun Fact:
Did you know your gut is often called your "second brain" because it contains over 100 million neurons—more than your spinal cord? This gut-brain connection is a key factor in Metabolic Chaos®, where poor gut health can trigger brain fog, mood swings, and hormonal imbalances. With over 70% of your immune system residing in your gut, it plays a crucial role in your overall health. Addressing gut health can unravel Metabolic Chaos® and create a ripple effect that restores balance to your entire body!
Breaking the Cycle of Trial and Error
If you’ve been stuck in the exhausting cycle of trying different treatments, diets, or supplements without success, it’s time to try a new approach. Metabolic Chaos® helps us move beyond simply managing symptoms to truly understanding the root cause of dysfunction. This holistic, individualized approach allows for long-term healing and the ability to regain control of your health.
Conclusion: Take the First Step Towards Healing
Your body is telling you something with every symptom—whether it’s fatigue, digestive issues, hormonal imbalances, or unexplained weight gain. These signs are part of a larger puzzle, and understanding Metabolic Chaos® is the key to putting the pieces together. By uncovering the root causes of your health challenges, we can create a roadmap to healing that restores balance and brings lasting vitality.
Ready to discover how Metabolic Chaos® may be affecting your health? I invite you to schedule a complimentary discovery call. Together, we’ll explore your unique health picture and begin the journey to uncover the hidden causes of your symptoms—empowering you to finally take control of your health and feel your best.
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Understanding Lab Ranges: Why You May Still Feel Unwell Even if Your Labs Are “Normal”
Understanding Lab Ranges: Why You May Still Feel Unwell Even if Your Labs Are “Normal”
In the world of traditional naturopathy and Functional Diagnostic Nutrition® (FDN), we take a unique approach to lab work. Our approach digs deeper than conventional medicine's standard lab ranges, aiming to help you achieve true vitality rather than simply existing within broad "normal" ranges. This article will break down the differences between standard and functional lab ranges and explain how they contribute to a more personalized, proactive healthcare approach.
The Difference Between Standard and Functional Lab Ranges
Standard Lab Ranges
Cholesterol: In conventional labs, total cholesterol levels are often considered normal if they fall within the range of 125-199 mg/dL. However, this range doesn’t account for individual differences in heart disease risk, inflammatory markers, or lifestyle factors. For instance, two individuals with cholesterol levels of 195 mg/dL might be classified as "normal" by standard labs, even if one has a family history of cardiovascular disease or other risk factors.
Thyroid-Stimulating Hormone (TSH): Standard TSH ranges can vary widely, but they are generally between 0.40-4.50 mIU/L in conventional labs. This broad range may overlook subclinical thyroid issues, especially if TSH is, say, at 4.8 mIU/L. Such values might indicate mild hypothyroid symptoms like fatigue, cold intolerance, or weight gain, but they are often dismissed as “normal” in conventional settings.
Fasting Glucose: Conventional labs usually set a normal fasting glucose range at 65-99 mg/dL. A level of 97 mg/dL would be considered “normal,” even though it might indicate early insulin resistance. Many people with glucose in the high end of this range already experience energy dips, weight gain, or cravings, showing signs of metabolic dysregulation.
Functional Lab Ranges
In Functional Diagnostic Nutrition® (FDN) and naturopathic practices, lab values are assessed using narrower, optimized ranges that are often more sensitive to early imbalances. These functional ranges identify healing opportunities rather than waiting for serious imbalances to appear. Here’s how these functional ranges compare:
Cholesterol: Functional ranges for total cholesterol are often more specific, typically ranging from 160-199 mg/dL for optimal heart health and inflammatory balance. Levels above or below this range might prompt a deeper investigation into diet, lifestyle, or genetic risk factors, even if they fall within conventional limits.
Thyroid-Stimulating Hormone (TSH): Functional ranges for TSH usually fall between 1.0-2.0 mIU/L. A TSH level of 4.5, although “normal” by conventional standards, would signal a potential hypothyroid tendency in functional health. Addressing this early could help prevent or reduce symptoms and avoid progression into more significant thyroid dysfunction.
Fasting Glucose: Functional health often defines an optimal fasting glucose range of 75-86 mg/dL. Even a level of 95 mg/dL, which is normal by conventional standards, could indicate insulin sensitivity issues in functional medicine. Identifying this early allows us to work on blood sugar stabilization through diet, exercise, and other lifestyle measures, reducing the risk of progressing to type 2 diabetes.
Data and Supporting Statistics
🌿 Thyroid Disorders: Studies have shown that subclinical hypothyroidism (characterized by a slightly elevated TSH within the "normal" range) affects approximately 4-8% of the general population. These individuals may experience symptoms like fatigue and weight gain, which often go unaddressed in conventional settings but could benefit from functional approaches.
🌿 Insulin Resistance: A study published in Diabetes Care found that up to 50% of people with fasting glucose levels at the high end of the "normal" range (90-99 mg/dL) developed prediabetes within ten years. Functional ranges would recognize these individuals as at-risk earlier, allowing for lifestyle changes to improve blood sugar stability.
🌿 Cholesterol and Heart Health: According to the American Heart Association, even individuals with "borderline" cholesterol (between 180-200 mg/dL) have an increased risk of cardiovascular issues, especially if they have additional risk factors. Functional practitioners would aim to optimize cholesterol within a tighter range, taking a more preventive approach.
By identifying these healing opportunities, we help clients understand how even “normal” lab results can signal underlying imbalances. Functional lab ranges give us a roadmap to achieve true health rather than waiting for symptoms to worsen.
The Value of Proactive Healthcare
Traditional medicine often takes a reactive approach—intervening only when a lab marker has crossed into an alarming range. But by using functional lab ranges, we work to be proactive rather than reactive. We aim to help you address early signs of imbalance or metabolic chaos® that may contribute to health problems over time. For example, someone may have blood sugar levels considered “normal” by conventional standards but still show signs of insulin resistance when examined through functional lenses. Addressing this earlier may help avoid more severe conditions like type 2 diabetes down the line.
Why “Normal” Isn’t Enough: Listening to Your Body
We understand the frustration when you're told your labs look “normal,” yet you continue to feel unwell. This is where working with a Traditional Naturopath and Certified FDN Practitioner can make a real difference. By focusing on functional lab ranges, we don’t overlook the symptoms you’re experiencing. Instead, we use tools like Optimal DX software to dig into your results in a meaningful way, creating an individualized health report and plan to address your unique needs. This software allows us to interpret your lab work through a functional health lens, identifying areas needing attention and recommending targeted nutraceuticals, diet changes, and lifestyle adjustments.
Fun Fact:
Did you know that in functional health, your body can start showing signs of imbalance long before they appear on standard lab tests? By looking at narrower, optimal ranges, functional practitioners often catch potential issues early, which can prevent bigger health problems down the road! It's like having a wellness crystal ball 🔮 for proactive health.
The Benefits of Individualized Care
When working with functional ranges, we create a personalized approach, taking into account your symptoms, lifestyle, and health history. Every recommendation is tailored to support your body’s unique needs, whether that means incorporating specific nutrients, dietary adjustments, or lifestyle changes.
Our ultimate goal is not only to help you avoid disease but to feel truly healthy and vibrant. By identifying root causes and addressing them holistically, we work together to restore optimal health and wellbeing.
Make Proactive Health Choices Today
Don’t wait for symptoms to worsen or rely solely on broad “normal” lab ranges that may overlook key healing opportunities. Schedule a consultation today to explore a functional approach to your health. With a proactive mindset and personalized support, we’ll help you understand what’s going on in your body and take steps toward a more vibrant, balanced life.
References
Optimal Lab Ranges vs. Standard Lab Ranges
Source: Lab Testing and Functional Ranges - Institute for Functional Medicine (IFM)
Website: https://www.ifm.org
Understanding Metabolic Chaos® in Functional Health
Source: Reed Davis, Founder of Functional Diagnostic Nutrition® - What is Metabolic Chaos®?
Website: https://fdntraining.com
Optimal DX Software for Individualized Lab Analysis
Source: Using Optimal DX to Improve Health Outcomes - Optimal DX
Website: https://optimaldx.com
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
The Vital Role of Sleep in Women's Health: From Puberty to Menopause and Beyond
The Vital Role of Sleep in Women's Health: From Puberty to Menopause and Beyond
In today’s fast-paced world, many women overlook the true importance of sleep, sacrificing precious hours to meet daily demands. However, sleep is fundamental for health, longevity, and quality of life, especially for women, whose sleep needs differ significantly from men’s. Research has shown that most adults, particularly women, need about 10 hours of sleep each night—not the standard 7-8 hours that’s often recommended. Many existing studies on sleep requirements have focused largely on men, making these recommendations inadequate for women. From puberty to menopause and beyond, sleep needs and patterns evolve throughout a woman's life. Without sufficient rest, women face unique health risks and challenges.
The Importance of Sleep for Women: Hormones, Health, and Vitality
Getting adequate sleep is foundational for hormone health, which regulates almost every system in the body. For women, this is especially important because hormonal shifts influence each life stage, from puberty through menopause. When women don’t get sufficient rest, they face a cascade of potential health issues affecting mood, immunity, weight, metabolism, and even fertility.
Research indicates that women often need more sleep than men, as the female brain requires additional energy to support multitasking, problem-solving, and cognitive recovery. Sleep restores this energy and bolsters cognitive function and emotional balance—essential for women managing multiple responsibilities.
Sleep is crucial for physical restoration, emotional regulation, cognitive clarity, and metabolic balance. It fosters hormonal harmony, supports immune health, enhances fertility, and aids in healthy aging. Chronic sleep deprivation disrupts nearly every system in the body, heightening the risk of serious health concerns. Among these, heart disease, obesity, type 2 diabetes, depression, and anxiety are particularly common in women lacking adequate sleep, impacting their longevity and quality of life.
How Hormones Impact Sleep from Puberty to Postmenopause
Sleep patterns shift throughout a woman’s life, fluctuating with hormonal transitions, each impacting sleep quality and quantity in unique ways. Here’s a look at how sleep evolves as women move through different life stages:
Puberty to Early Adulthood:
At the onset of puberty, hormonal changes, especially increases in estrogen and progesterone, can disrupt sleep patterns, often causing later bedtimes and morning sluggishness. Quality sleep during these formative years is essential for mood regulation, brain development, and reproductive health, as it helps balance hormones necessary for these functions.
Reproductive Years and Fertility:
During a woman’s reproductive years, sleep supports balanced estrogen, progesterone, and other hormones crucial for fertility and reproductive health. Poor sleep can interfere with ovulation and increase the risk of conditions like polycystic ovary syndrome (PCOS), which can complicate fertility. Good sleep is essential for hormone regulation, reducing stress hormones, and supporting a stable menstrual cycle.
Perimenopause: “Puberty in Reverse”:
As women transition to menopause, also known as perimenopause, estrogen and progesterone levels begin to fluctuate significantly—much like “puberty in reverse.” This phase often brings sleep disturbances, including night sweats, hot flashes, and insomnia, which fragment sleep, making it difficult to get a full night’s rest. Fluctuating hormone levels can also heighten stress responses, further impacting sleep quality.
Menopause and Beyond:
After menopause, lower estrogen levels can continue to affect sleep, often leading to increased wakefulness during the night and earlier awakenings. Lower estrogen impacts melatonin production, the hormone that regulates sleep-wake cycles, and can also contribute to a decrease in overall sleep quality. Quality sleep during these years is essential for mental clarity, immune function, and bone health, as well as for reducing the risk of chronic diseases.
The Sleep-Hormone Connection: A Lifelong Relationship
Hormones such as estrogen, progesterone, cortisol, and melatonin are deeply intertwined with sleep patterns and quality. For example, high cortisol levels, often resulting from chronic stress, can make it difficult to fall or stay asleep. Low melatonin levels, which naturally decrease with age and can be impacted by hormonal changes, disrupt the body’s circadian rhythm, affecting the depth and restorative quality of sleep.
Hormonal shifts during key life stages like puberty, pregnancy, perimenopause, and menopause bring changes in sleep patterns for many women. These shifts underscore the critical link between sleep and hormone health, showing how sleep supports not only physical restoration but also emotional stability, cognitive clarity, and metabolic balance throughout a woman’s life.
Natural Strategies for Better Sleep
To support your natural sleep rhythms, try the following holistic strategies:
🌿 Herbal Remedies: Valerian root, chamomile, and passionflower can be gentle but effective sleep aids. These herbs help relax the body and ease stress, improving sleep quality.
🌿 Vitamins and Minerals: Magnesium, vitamin D, and B vitamins play essential roles in sleep regulation. Magnesium, for instance, can help calm the nervous system and ease muscle tension, which may help you fall asleep faster.
🌿 Whole-Food, Plant-Based Diet: Avoiding processed foods, sugars, and ca ffeine late in the day while focusing on whole foods rich in fiber, healthy fats, and protein can help balance blood sugar levels and stabilize energy, reducing nighttime disturbances.
🌿 Exercise: Regular, moderate exercise helps lower stress hormones and improve sleep quality. Be mindful to exercise at least a few hours before bed to avoid overstimulation.
🌿 Sleep Hygiene: Maintain a regular sleep schedule, keep your bedroom cool and dark, and avoid screens at least an hour before bedtime. Try to create a relaxing pre-sleep routine, like reading or gentle stretching.
🌿 Stress Management: Meditation, deep breathing exercises, and mindfulness practices can all reduce stress, improving your body’s ability to relax before bed.
Why Sleep is Often Disrupted for Women: Perimenopause and Beyond
Sleep quality can be affected by a range of factors unique to women, particularly as they enter perimenopause and beyond. Hormonal changes, life stressors, and lifestyle choices all contribute to sleep challenges at various life stages.
Hormonal Shifts During Perimenopause and Menopause
During perimenopause and menopause, declining levels of estrogen and progesterone can significantly disrupt sleep. Estrogen plays a key role in regulating body temperature and melatonin production, so as estrogen levels drop, women may experience night sweats, hot flashes, and insomnia. Progesterone, a hormone with calming effects, also decreases, making it harder to relax and fall asleep. These hormone-related sleep disruptions often lead to sleep fragmentation, reducing overall sleep quality.
Life Stressors
Stress from balancing work, family, and unexpected life changes can keep women awake, affecting both the quantity and quality of their sleep. Chronic stress elevates cortisol levels, which can make it difficult to wind down at night, setting off a cycle of sleep difficulties that affect physical and emotional well-being.
Pregnancy and Motherhood
Pregnancy and caring for an infant come with their own sleep challenges. Physical discomfort, hormonal shifts, and frequent nighttime awakenings with a newborn often result in interrupted sleep, impacting a mother’s overall health and hormone balance.
Increased Susceptibility to Sleep Disorders
Women are more likely than men to experience certain sleep disorders, including insomnia, sleep apnea, and restless leg syndrome. Hormonal changes can heighten the risk of these conditions, especially during perimenopause and menopause, as estrogen and progesterone fluctuations impact respiratory stability, muscle tone, and overall sleep architecture.
Diet and Lifestyle Factors
Diet and lifestyle choices also play a significant role in sleep quality. Eating too late, consuming excess caffeine or alcohol, and maintaining an inconsistent sleep schedule can all negatively impact the ability to fall and stay asleep. These habits can disrupt circadian rhythms and interfere with deep, restorative sleep, making it even more challenging for women to achieve the restful sleep they need.
Each of these factors highlights the complex relationship between hormonal balance, lifestyle, and sleep. For women, understanding and addressing these disruptions is key to achieving restful sleep, particularly as they navigate perimenopause, menopause, and beyond.
Fun Fact:
Humans are the only mammals that willingly delay sleep! Unlike animals, which tend to fall asleep whenever they're tired, humans often stay up past when their bodies naturally want to sleep—thanks to artificial lights, entertainment, and other activities. So if you've ever found yourself binging a series late at night, you’re tapping into a very "human" behavior!
Testing for Sleep Quality: Getting to the Root of Sleep Issues
Understanding the root causes of sleep issues requires thorough evaluation. Here are some ways to assess sleep health:
Blood, Saliva, and Urine Testing: Hormone levels, including cortisol, melatonin, estrogen, and progesterone, can be evaluated to understand imbalances that affect sleep.
Sleep Study: This test assesses brain wave activity, oxygen levels, and other factors, providing a comprehensive view of sleep quality.
DNAlife and DUTCH Plus Tests: These advanced tests provide valuable insights into sleep-related genes like the CLOCK gene, which influences circadian rhythms. They also assess cortisol patterns, helping to pinpoint issues with adrenal function that may disrupt sleep.
Sleep and Hormone Health: Why They’re So Connected
Sleep is a crucial aspect of hormonal balance. Disrupted sleep affects cortisol, estrogen, progesterone, and melatonin, creating a cascade of hormonal imbalances. The CLOCK gene plays a role in regulating our biological rhythms and can influence how well a woman responds to various sleep support strategies. Identifying any genetic predispositions or hormonal imbalances is key to optimizing sleep.
Final Thoughts: Prioritize Your Sleep for Lasting Health
For women, sleep is not just a time to rest; it’s a time for the body to heal, recharge, and regulate critical hormones. By taking steps to improve sleep quality naturally and seeking appropriate testing when needed, you can create a foundation for better overall health. Invest in your sleep—it’s one of the most powerful forms of self-care that you can give yourself.
Sleep well, stay balanced, and remember that quality sleep is key to a healthier, more vibrant you!
Preferences
Hormonal Changes and Sleep Disturbances in Perimenopause and Menopause
Source: "Menopause and Sleep" – Sleep Foundation
Website: Sleep Foundation
Stress and Cortisol's Impact on Sleep
Source: "How Stress Affects Sleep" – American Psychological Association (APA)
Website: APA on Stress and Sleep
Sleep Disorders in Women
Source: "Sleep Disorders in Women" – Office on Women’s Health, U.S. Department of Health and Human Services
Website: Office on Women’s Health
Impact of Melatonin and Estrogen on Sleep
Source: "Hormones and Sleep" – National Institute on Aging
Website: National Institute on Aging
Diet, Lifestyle, and Sleep Quality
Source: "Diet, Lifestyle and Sleep Health" – Harvard T.H. Chan School of Public Health
Website: Harvard School of Public Health
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Progesterone: Nature’s Xanax and the Unsung Hero of Women’s Health
Progesterone: Nature’s Xanax and the Unsung Hero of Women’s Health
When we think about hormones, estrogen often steals the spotlight, but progesterone deserves just as much attention, if not more. Known as nature’s Xanax for its calming effects, progesterone is crucial to a woman’s well-being—from puberty to menopause and beyond. Here’s a closer look at what makes this hormone so powerful and how to support balanced progesterone levels naturally.
What is Progesterone, and How is it Made?
Progesterone is a steroid hormone primarily produced in the ovaries after ovulation, but it’s also made in smaller amounts by the adrenal glands. It stems from a parent hormone called pregnenolone, which is synthesized from cholesterol. This process highlights how essential healthy fats are in our diet, as they’re the building blocks of our vital hormones.
Progesterone’s Role in a Woman’s Life Cycle
Puberty and Fertility
During puberty, our bodies prepare for reproductive health. Progesterone, alongside estrogen, is essential in regulating the menstrual cycle, supporting a regular and healthy cycle. In terms of fertility, progesterone has the critical job of preparing the uterus for pregnancy. Without adequate levels, it’s challenging to conceive, as progesterone maintains a nurturing environment in the uterus for a fertilized egg to implant and grow.
Perimenopause: Puberty in Reverse
As we approach perimenopause, it’s almost like experiencing “puberty in reverse.” This stage, which typically begins in our 40s but can happen earlier, sees a natural decline in progesterone levels. This transition can last several years until menopause, the point when menstrual cycles stop entirely. Low progesterone during perimenopause often results in mood swings, irregular cycles, and sleep issues.
Menopause and Beyond
Even after menopause, when estrogen and progesterone levels have dropped significantly, the balance between these two hormones remains important. A stable hormonal balance can help protect our bones, support heart health, and even impact our brain function as we age.
Natural Ways to Boost Progesterone Levels
While progesterone levels naturally decline with age, lifestyle practices can help maintain a healthy balance:
🌿 Herbal Remedies: Vitex (chasteberry) is often used to support progesterone production. Maca root, a powerhouse adaptogen, can also help balance overall hormones.
🌿 Nutritional Support: Certain nutrients, including vitamin B6, magnesium, and zinc, play crucial roles in progesterone production. A diet rich in whole, plant-based foods, including leafy greens, legumes, nuts, and seeds, can supply these nutrients.
🌿 Diet: A whole food, plant-based diet supports hormone health by reducing inflammation and balancing blood sugar levels. Healthy fats, like those found in avocados, olive oil, and nuts, are also essential for hormone production.
🌿 Exercise: Regular, moderate exercise helps reduce stress and supports hormonal balance, but too much high-intensity exercise can have the opposite effect. Balance is key.
🌿 Sleep and Stress Management: Progesterone has a calming effect on the brain. Prioritizing quality sleep and managing stress through practices like mindfulness, deep breathing, or stretching can support progesterone levels.
Hormone Therapy Options
For some women, lifestyle changes may not be enough. Bioidentical Hormone Replacement Therapy (BHRT) and compounded bioidentical hormone replacement therapy (cBHRT) are options that mimic the body’s natural hormones, which can help regulate progesterone levels and ease the symptoms of perimenopause and menopause. These options should be considered with a healthcare provider who can create a customized plan based on individual hormone levels and symptoms.
Testing for Hormone Balance: Blood, Saliva, and Urine
Monitoring progesterone levels and overall hormone health can provide valuable insight into what your body needs. There are different tests available:
Blood (Serum) Test: Measures the levels of free hormones circulating in the bloodstream, often used as a first-line measure.
Saliva Test: Measures the free hormone levels as well and is useful for assessing bioavailable hormone levels, though it’s not as comprehensive for some.
DUTCH (Dried Urine Test for Comprehensive Hormones): This advanced test shows a complete picture of how your body metabolizes hormones. It can be particularly valuable for understanding hormonal patterns throughout the day and is often used alongside blood tests for a fuller picture of hormone function and imbalance.
Using both a serum and DUTCH test can be extremely helpful for women looking to balance hormones naturally or through hormone replacement therapy. Together, they provide a comprehensive view, helping practitioners fine-tune treatment and monitor changes over time.
Progesterone: Nature’s Xanax
Progesterone’s nickname, “nature’s Xanax,” highlights its calming effects on the brain and nervous system. It helps regulate mood, promotes relaxation, and supports restful sleep—making it especially important during perimenopause, when fluctuations can lead to anxiety, irritability, and insomnia. Balancing progesterone can feel like rediscovering a sense of calm amidst the turbulence of hormonal shifts.
When to Start Paying Attention to Progesterone
It’s never too early to think about hormone health, but many women start focusing on progesterone around their mid-30s or early 40s, as signs of perimenopause begin to appear. Working with a healthcare provider to test and monitor hormone levels allows you to take proactive steps to maintain balance and support your body through each life stage.
Fun Fact:
Did you know that progesterone is not just a “female” hormone? Men produce small amounts of progesterone, too! It plays a role in balancing their estrogen levels and even supports brain health. So, while women rely on it much more, this calming hormone benefits everyone.
Final Thoughts: Supporting Progesterone for a Balanced Life
Hormones have an incredible impact on our mental, emotional, and physical well-being, and progesterone plays a vital role in achieving that balance. By adopting a lifestyle that prioritizes sleep, healthy nutrition, stress management, and regular testing, you can support your body’s natural production of this essential hormone. If you’re experiencing symptoms that impact your quality of life, consider working with a healthcare professional to discuss natural support, hormone replacement options, and appropriate testing.
Call to Action: Embrace Balance, Embrace Vitality
Hormone balance isn’t just about managing symptoms—it’s about enhancing vitality and well-being. By taking steps to understand and support your body’s unique hormonal needs, you can create a more balanced, peaceful, and energized life at any age. Ready to take control of your hormonal health? Start by exploring testing options and contact us today so we can guide you through your unique journey.
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
The Case Against Alcohol: A Functional Medicine Perspective
The Case Against Alcohol: A Functional Medicine Perspective
Alcohol consumption is a common part of social gatherings, celebrations, and even daily routines for many. However, as a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner and someone who upholds the Seventh-day Adventist commitment to holistic health, I believe it's essential to examine the impact of alcohol on our bodies, minds, and spirits. This article will explore the reasons why avoiding alcohol is beneficial, from a biblical, scientific, and functional medicine standpoint, and offer guidance on how to support your body if you choose to abstain.
Biblical Perspective: A Call to Holiness
As Seventh-day Adventists, we are called to live lives that honor God, including taking care of our bodies as temples of the Holy Spirit. The Bible contains several warnings about the dangers of alcohol. Proverbs 20:1 (NIV) says, “Wine is a mocker and beer a brawler; whoever is led astray by them is not wise.” Furthermore, in 1 Corinthians 6:19-20, we are reminded that our bodies are temples of the Holy Spirit and that we are to glorify God with our bodies.
While the Bible doesn’t explicitly forbid alcohol, the only permissible use is for the medicinal purposes, Proverbs 31:6 (CEV) Beer and wine are only for the dying or for those who have lost all hope. The negative impacts of alcohol are well-documented, and avoiding it aligns with a lifestyle of holiness and respect for the body God has given us.
Scientific Evidence Against Alcohol Consumption
From a functional medicine perspective, the effects of alcohol on health are significant and concerning. Scientific research over the decades has revealed significant negative health impacts of alcohol, even at moderate consumption levels. Here’s a deeper look into the scientific evidence against alcohol consumption and its effects on various aspects of health.
Liver Health: The Primary Organ Affected by Alcohol
The liver is the body's main detoxifying organ, responsible for metabolizing substances, including alcohol. When you consume alcohol, the liver works to break it down into acetaldehyde, a toxic compound, which is then further metabolized into less harmful substances that the body can eliminate. Chronic alcohol consumption overwhelms the liver's capacity to process alcohol, leading to a variety of liver-related health issues:
Fatty Liver Disease: Also known as hepatic steatosis, this condition involves the accumulation of fat in liver cells. Even light to moderate alcohol intake can lead to this condition if consumed regularly over time. Fatty liver is reversible with abstinence but can progress to more severe liver diseases if alcohol consumption continues.
Alcoholic Hepatitis: This inflammatory condition occurs due to prolonged alcohol exposure, leading to liver cell injury and inflammation. Symptoms include jaundice, abdominal pain, and fever. Severe cases can be life-threatening and often require medical intervention.
Cirrhosis: This is the final stage of chronic liver disease and is characterized by the irreversible scarring of liver tissue. Cirrhosis greatly increases the risk of liver failure and liver cancer. Studies have shown that heavy drinking over many years can lead to cirrhosis, but even moderate drinking has been associated with an increased risk.
A comprehensive review published in the Journal of Hepatology highlighted that alcohol-related liver disease accounts for more than half of liver disease deaths in the United States, indicating the significant burden alcohol places on liver health (Seitz et al., 2018).
Brain Health: Long-Term Impacts on Cognitive Function
Alcohol affects the brain in multiple ways, both in the short term (intoxication) and long term (neurodegeneration). Here’s how alcohol impacts brain health:
Neurotoxicity: Alcohol is a neurotoxin, meaning it damages brain cells. Chronic alcohol consumption can lead to a reduction in brain volume, particularly in the frontal lobe, which is responsible for executive functions such as decision-making, problem-solving, and impulse control. Research published in the BMJ found that even moderate drinking was associated with an increased risk of brain volume reduction and cognitive decline (Topiwala et al., 2017).
Memory and Learning: Alcohol particularly affects the hippocampus, the brain region critical for memory and learning. Studies have shown that heavy drinking can lead to shrinkage of the hippocampus, contributing to memory impairments and an increased risk of developing conditions like Alzheimer's disease (Sullivan et al., 2010).
Mental Health: Alcohol consumption has been linked to various mental health disorders, including depression and anxiety. The relationship is bidirectional; alcohol can exacerbate mental health issues, and people with mental health issues are more likely to consume alcohol. A meta-analysis published in Addiction indicated that alcohol use disorder (AUD) is associated with an increased risk of major depression and anxiety disorders (Boden & Fergusson, 2011).
Increased Cancer Risk: Alcohol as a Carcinogen
Alcohol has been classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC), meaning it is known to cause cancer in humans. Here’s how alcohol contributes to cancer development:
Mechanisms of Carcinogenesis: Alcohol metabolism produces acetaldehyde, a toxic substance that can damage DNA and proteins. Acetaldehyde can interfere with the repair of damaged DNA, increasing the likelihood of mutations that can lead to cancer. Additionally, alcohol can increase levels of estrogen and other hormones associated with breast cancer.
Types of Cancer: Alcohol consumption has been linked to several types of cancer, including but not limited to:
Breast Cancer: Even low levels of alcohol intake (as little as one drink per day) can increase the risk of breast cancer in women. A pooled analysis of data from multiple studies found a clear dose-response relationship between alcohol intake and breast cancer risk (Chen et al., 2011).
Liver Cancer: Chronic alcohol consumption is a major risk factor for hepatocellular carcinoma, the most common type of liver cancer. The link between alcohol and liver cancer is largely due to alcohol-induced cirrhosis.
Colorectal Cancer: Alcohol consumption has been associated with an increased risk of colorectal cancer. A meta-analysis published in the American Journal of Epidemiology found that individuals who consumed more than 50 grams of alcohol per day (approximately four drinks) had a significantly increased risk of colorectal cancer (Cho et al., 2004).
Impact on Gut Health: The Microbiome and Beyond
The gut microbiome plays a critical role in overall health, influencing digestion, immune function, and even mental health. Alcohol disrupts the balance of the gut microbiome, leading to dysbiosis—a condition characterized by an imbalance between beneficial and harmful bacteria in the gut.
Leaky Gut Syndrome: Alcohol can damage the intestinal lining, leading to increased intestinal permeability or "leaky gut." This condition allows toxins and bacteria to pass from the gut into the bloodstream, triggering systemic inflammation. Chronic inflammation is a key driver of many chronic diseases, including autoimmune disorders and metabolic syndrome (Wang et al., 2010).
Digestive Issues: Alcohol can increase gastric acid secretion and delay gastric emptying, leading to conditions like acid reflux, gastritis, and peptic ulcers. Chronic alcohol use can also impair nutrient absorption, contributing to deficiencies in essential vitamins and minerals.
Genetic Predispositions: Understanding Individual Risks
Not everyone responds to alcohol in the same way, and genetics play a significant role in determining how alcohol affects an individual. Genetic variations can influence how efficiently the body metabolizes alcohol, which can affect a person's risk of developing alcohol-related health problems.
ADH1B and ALDH2 Genes: These genes encode enzymes involved in alcohol metabolism. Variants of these genes can lead to slower metabolism of acetaldehyde, resulting in a buildup of this toxic substance. Individuals with certain genetic variants are more likely to experience adverse effects from alcohol, including an increased risk of liver disease and cancer. Research published in Human Genetics discusses how genetic testing can help identify individuals at higher risk of alcohol-related health issues, allowing for more personalized health recommendations (Hurley & Edenberg, 2012) .
Fun Fact about Sobriety:
Did you know that there is a growing trend called "Sober Curious"? This movement encourages people to explore and question their drinking habits, even if they don’t identify as having a drinking problem. The idea is to experiment with sobriety, whether it's for a night, a week, a month, or more, and see how cutting out alcohol affects their mental clarity, mood, sleep, and overall well-being. Many people who try being "sober curious" report feeling more energized, focused, and connected to their surroundings, which shows that choosing sobriety can bring unexpected and positive changes to your life!
Nutrients and Botanicals to Support Sobriety: A Scientific Approach
Achieving and maintaining sobriety from alcohol can be a challenging journey that involves not only breaking the cycle of dependence but also healing the body from the effects of chronic alcohol use. Nutrients and botanicals can play a crucial role in supporting this process by helping to repair damage, alleviate withdrawal symptoms, and promote overall health. Here’s a detailed look into the scientific evidence behind some of the most effective nutrients and botanicals for supporting sobriety.
B Vitamins: Vital for Brain and Nervous System Health
B vitamins, particularly thiamine (B1), folate (B9), and vitamin B12, are critical for brain health and neurological function. Chronic alcohol consumption often leads to deficiencies in these vitamins due to poor dietary intake, impaired absorption, and increased excretion.
Thiamine (Vitamin B1): Alcohol interferes with the absorption of thiamine and its conversion to its active form. Thiamine deficiency can lead to Wernicke-Korsakoff syndrome, a serious neurological condition characterized by confusion, memory loss, and motor dysfunction. Supplementing with thiamine can help prevent or reduce the severity of this syndrome in recovering alcoholics (Day et al., 2013). Regular intake of thiamine is also associated with improved energy metabolism and cognitive function, which are often impaired in those recovering from alcohol dependence.
Folate (Vitamin B9) and Vitamin B12: These vitamins are essential for DNA synthesis, repair, and methylation, processes that are often disrupted in alcoholics due to poor diet and malabsorption. Folate deficiency is particularly common in individuals with alcohol use disorder and is linked to cognitive impairment and mood disorders. Supplementation with folate and B12 has been shown to improve mood and cognitive function in recovering alcoholics (Miller, 2008).
Omega-3 Fatty Acids: Anti-inflammatory and Neuroprotective
Omega-3 fatty acids, particularly EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), are essential fats that have powerful anti-inflammatory and neuroprotective effects. They are crucial for brain health, reducing inflammation, and supporting cell membrane integrity.
Inflammation Reduction: Chronic alcohol consumption leads to systemic inflammation, which can damage various organs, including the brain. Omega-3 fatty acids have been shown to reduce inflammation by inhibiting the production of pro-inflammatory cytokines and promoting the resolution of inflammation (Calder, 2013). This anti-inflammatory effect can be particularly beneficial in reducing the risk of neurodegenerative diseases and cognitive decline associated with chronic alcohol use.
Neuroprotection: Omega-3s support brain health by enhancing neuronal membrane fluidity, which is crucial for proper neurotransmitter function and synaptic plasticity. Studies have shown that omega-3 supplementation can improve cognitive function and reduce the risk of depression in recovering alcoholics, potentially by modulating neurotransmitter pathways and reducing oxidative stress (Sontrop & Campbell, 2006).
Magnesium: Restoring Cellular Function and Reducing Anxiety
Magnesium is an essential mineral involved in over 300 enzymatic reactions in the body, including those related to energy production, DNA synthesis, and nerve transmission. Chronic alcohol use is known to deplete magnesium levels, which can lead to symptoms such as fatigue, muscle cramps, anxiety, and insomnia.
Anxiety Reduction: Magnesium plays a critical role in modulating the body's stress response and has been shown to have a calming effect on the nervous system. Studies have demonstrated that magnesium supplementation can reduce anxiety and improve sleep quality in individuals with alcohol use disorder, potentially by modulating the HPA (hypothalamic-pituitary-adrenal) axis and neurotransmitter activity (Boyle et al., 2017).
Cellular Function: Magnesium is also crucial for maintaining cellular function and energy production. By supporting ATP (adenosine triphosphate) production and stabilizing cellular membranes, magnesium can help restore energy levels and reduce fatigue in individuals recovering from alcohol dependence.
N-Acetylcysteine (NAC): Antioxidant and Glutathione Support
N-Acetylcysteine (NAC) is a precursor to glutathione, the body’s most potent antioxidant. NAC is known for its ability to replenish intracellular levels of glutathione, thereby protecting cells from oxidative stress and reducing inflammation.
Antioxidant Protection: Chronic alcohol consumption increases oxidative stress, leading to cell damage and contributing to liver disease, brain damage, and other alcohol-related health issues. NAC has been shown to reduce oxidative stress by boosting glutathione levels, thereby protecting cells from damage. In the context of alcohol recovery, NAC supplementation can help mitigate the oxidative damage caused by long-term alcohol use (Amini et al., 2018).
Liver Support: NAC is also used as a treatment for acetaminophen poisoning, which can cause acute liver failure. This application underscores its potential to protect liver cells from damage. In recovering alcoholics, NAC can support liver health by promoting detoxification and reducing liver inflammation (Samuni et al., 2013).
Milk Thistle (Silybum marianum): Liver Detoxification and Protection
Milk thistle is a botanical known for its liver-protective properties, largely due to its active compound, silymarin. Silymarin has antioxidant, anti-inflammatory, and antifibrotic effects, making it beneficial for liver health.
Liver Detoxification: Silymarin helps to enhance liver detoxification pathways by increasing the levels of glutathione and superoxide dismutase, two critical antioxidants in liver detoxification. This enhancement helps to protect liver cells from oxidative damage caused by alcohol metabolism (Abenavoli et al., 2018).
Liver Regeneration: Research has shown that milk thistle can promote the regeneration of liver tissue and improve liver function in individuals with liver diseases, including those related to alcohol consumption. A systematic review concluded that milk thistle supplementation could improve liver enzyme levels and reduce the symptoms of liver disease in patients with alcoholic liver disease (Loguercio & Festi, 2011).
Kudzu (Pueraria lobata): Reducing Alcohol Cravings
Kudzu is an herb traditionally used in Chinese medicine that has gained attention for its potential to reduce alcohol cravings and consumption.
Craving Reduction: The active compounds in kudzu, such as puerarin, have been shown to affect neurotransmitter systems in the brain, particularly those involving dopamine and serotonin. Studies suggest that kudzu can reduce alcohol intake and delay the onset of intoxication by altering the way alcohol is metabolized and its effects on the brain (Keung & Vallee, 1998).
Supporting Abstinence: A small clinical trial found that individuals who took kudzu extract before drinking consumed less alcohol and showed lower levels of alcohol-related impairment than those who took a placebo. This suggests that kudzu may be a helpful botanical in supporting sobriety by reducing the desire to drink (Lukas et al., 2005).
Ashwagandha (Withania somnifera): Stress Reduction and Adrenal Support
Ashwagandha is an adaptogenic herb known for its ability to reduce stress and support adrenal function, which can be particularly beneficial during alcohol withdrawal and recovery.
Stress and Anxiety Reduction: Ashwagandha has been shown to reduce cortisol levels, a hormone associated with stress. By lowering cortisol, ashwagandha can help reduce anxiety and improve mood, which are common challenges faced by individuals in recovery from alcohol dependence (Chandrasekhar et al., 2012).
Adrenal Support: Chronic alcohol use can lead to adrenal fatigue, characterized by low energy, poor stress tolerance, and mood swings. Ashwagandha supports adrenal health by promoting balance in the body's stress response system, thereby helping to restore energy levels and improve resilience to stress (Singh et al., 2011).
Where to buy:
Gethealthy.store- US
Fullscript- US
Amrita Nutrition Uk- International code: KXCTGG
Amrita Nutrition Global- International code: 70FB2AB56158
Conclusion: Nourishing Your Path to Sobriety
Sobriety is not just about abstaining from alcohol; it’s about healing your body, mind, and spirit. Through the power of scientifically-backed nutrients and botanicals like B vitamins, omega-3s, magnesium, NAC, and herbs like milk thistle and kudzu, you can support your body's natural recovery processes. These nutrients help replenish what alcohol may have depleted, reduce cravings, protect vital organs, and restore balance to your life.
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I encourage you to take the first step in supporting your health and wellbeing. For those interested in understanding their personal risk factors for alcohol sensitivity or dependency, consider genetic testing through DNAlife. Genetic insights can empower you to make informed decisions about your health and create a personalized plan to support your sobriety journey.
Call to Action:
Nutrients and botanicals offer a powerful, scientifically-backed approach to supporting sobriety and recovery from alcohol dependence. By addressing nutritional deficiencies, reducing inflammation, supporting liver function, and helping to manage stress and cravings, these natural therapies can play a crucial role in the recovery process.
For individuals seeking to support their sobriety journey with targeted nutritional and botanical interventions, contact us so we can provide personalized guidance. Additionally, genetic testing through services like DNAlife can offer insights into individual predispositions and help tailor a more effective recovery plan.
Let’s craft a fab, healthy, and delicious non-alcoholic "wine" that you can sip and savor! 🍇✨ Here’s a recipe that mimics the taste of wine but keeps it light, fruity, and refreshing:
Sparkling Grape & Berry Wine Mocktail 🍷✨
Ingredients:
1 cup of 100% grape juice (red or white, your choice!)
½ cup of pomegranate juice (adds that rich, deep flavor)
A splash of lemon juice (for a bit of acidity)
½ cup of sparkling water (for those delightful bubbles)
Fresh berries (blueberries, raspberries, or strawberries work best)
A few sprigs of fresh mint (optional, but adds a lovely aroma)
Directions:
1. Chill your grape and pomegranate juices beforehand for a crisp, refreshing mocktail. ❄️
2. In a pitcher, combine the grape juice, pomegranate juice, and a small splash of lemon juice.
3. Gently muddle the fresh berries in the bottom of your glass (or skip this step if you like it smooth).
4. Pour the juice mixture into the glass, leaving some room at the top.
5. Top it off with sparkling water to give it that signature fizz.
6. Garnish with a few more berries and a sprig of mint. 🌿
🍇 Voila! You've got yourself a delightful, healthy mock "wine" perfect for sipping any time you want to feel a little fancy without the alcohol! 🍷🎉
Here’s a quick rundown of the health perks in your mock "wine":
Grape Juice: Rich in antioxidants (like resveratrol), which support heart health and boost immunity. 🍇
Pomegranate Juice: Packed with vitamin C and anti-inflammatory properties, it’s great for skin and heart health. ❤️
Lemon Juice: High in vitamin C, it aids digestion and helps detox the body. 🍋
Sparkling Water: Hydrates with a refreshing twist and no added sugars. 💧
Berries: Full of antioxidants, they improve brain health and fight inflammation. 🫐
Mint: Aids digestion and offers a refreshing, calming aroma. 🌱
Sip away, your health will thank you! 🌟
Citation:
Liver Health and Alcohol:
- Mayo Clinic. "Alcohol use: Weighing risks and benefits." Accessed August 12, 2024. [Mayo Clinic].
- Seitz, H. K., Bataller, R., Cortez-Pinto, H., Gao, B., Gual, A., Lackner, C., ... & Morgan, T. R. (2018). "Alcoholic liver disease." Journal of Hepatology, 69(4), 1104-1109. [Journal of Hepatology].
Brain Health and Alcohol:
- Harper, C. G., & Matsumoto, I. (2005). "Ethanol and brain damage." Current Opinion in Pharmacology, 5(1), 73-78. doi:10.1016/j.coph.2004.06.009 [Current Opinion in Pharmacology].
- Topiwala, A., Allan, C. L., Valkanova, V., Zsoldos, E., Filippini, N., Sexton, C., ... & Ebmeier, K. P. (2017). "Moderate alcohol consumption as risk factor for adverse brain outcomes and cognitive decline: longitudinal cohort study." BMJ, 357, j2353. [BMJ].
- Alcohol and Mental Health - Addiction:
- Boden, J. M., & Fergusson, D. M. (2011). "Alcohol and depression." Addiction, 106(5), 906-914. [Addiction].
Cancer Risk and Alcohol:
- World Health Organization. "Alcohol and Cancer." Accessed August 12, 2024. [WHO].
- American Cancer Society. "Alcohol Use and Cancer." Accessed August 12, 2024. [American Cancer Society].
- Chen, W. Y., Rosner, B., Hankinson, S. E., Colditz, G. A., Willett, W. C. (2011). "Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk." JAMA, 306(17), 1884-1890. [JAMA].
- Colorectal Cancer and Alcohol - American Journal of Epidemiology:
- Cho, E., Smith-Warner, S. A., Ritz, J., van den Brandt, P. A., Colditz, G. A., Folsom, A. R., ... & Hunter, D. J. (2004). "Alcohol Intake and Colorectal Cancer: A Pooled Analysis of 8 Cohort Studies." American Journal of Epidemiology, 159(7), 667-676. [American Journal of Epidemiology].
Gut Health and Alcohol:
- Leclercq, S., Matamoros, S., Cani, P. D., Neyrinck, A. M., Jamar, F., Stärkel, P., & de Timary, P. (2014). "Intestinal permeability, gut-bacterial dysbiosis, and behavioral markers of alcohol-dependence severity." Proceedings of the National Academy of Sciences, 111(42), E4485-E4493. [PNAS].
Genetic Predispositions and Alcohol Sensitivity:
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). "Genetics of Alcohol Use Disorder." Accessed August 12, 2024. [NIAAA].
- Hurley, T. D., & Edenberg, H. J. (2012). "Genes encoding enzymes involved in ethanol metabolism." Alcohol Research: Current Reviews, 34(3), 339-344. [Alcohol Research].
Citation: Nutrients and Botanicals to Support Sobriety
Day, E., Bentham, P., Callaghan, R., Kuruvilla, T., George, S. (2013). "Thiamine for prevention and treatment of Wernicke-Korsakoff Syndrome in people who abuse alcohol." Cochrane Database of Systematic Reviews. [Cochrane Library].
Miller, A. L. (2008). "The methylation, neurotransmitter, and antioxidant connections between folate and depression." Alternative Medicine Review, 13(3), 216-226. [Alternative Medicine Review].
Calder, P. C. (2013). "Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology?" British Journal of Clinical Pharmacology, 75(3), 645-662. [Journal].
Sontrop, J., & Campbell, M. K. (2006). "Omega-3 polyunsaturated fatty acids and depression: A review of the evidence and a methodological critique." Preventive Medicine, 42(1), 4-13. [ScienceDirect].
Boyle, N. B., Lawton, C., & Dye, L. (2017). "The Effects of Magnesium Supplementation on Subjective Anxiety and Stress—A Systematic Review." Nutrients, 9(5), 429. [MDPI Nutrients].
Amini, N., Fararouei, M., Akbarzadeh, A., Shamsi, F., Rajabzadeh, F., & Ghasemi, F. (2018). "Effect of N-acetylcysteine on liver function in patients with non-alcoholic fatty liver disease: A randomized clinical trial." European Journal of Gastroenterology & Hepatology, 30(1), 53-59. [Wolters Kluwer].
Samuni, Y., Goldstein, S., Dean, O. M., & Berk, M. (2013). "The chemistry and biological activities of N-acetylcysteine." Biochimica et Biophysica Acta (BBA) - General Subjects, 1830(8), 4117-4129. [ScienceDirect].
Abenavoli, L., Capasso, R., Milic, N., & Capasso, F. (2018). "Milk Thistle in Liver Diseases: Past, Present, Future." Phytotherapy Research, 32(2), 239-255. [Wiley Online Library].
Loguercio, C., & Festi, D. (2011). "Silybin and the liver: From basic research to clinical practice." World Journal of Gastroenterology, 17(18), 2288-2301. [World Journal of Gastroenterology].
Keung, W. M., & Vallee, B. L. (1998). "Kudzu root: An ancient Chinese source of modern antidipsotropic agents." Phytochemistry, 47(4), 499-506. [ScienceDirect].
Lukas, S. E., Penetar, D. M., Berko, J., Vicens, L., Palmer, C., Mallya, G., ... & Lee, D. Y. W. (2005). "An extract of the Chinese herbal root kudzu reduces alcohol drinking by heavy drinkers in a naturalistic setting." Alcoholism: Clinical and Experimental Research, 29(5), 756-762. [Wiley Online Library].
Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). "A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of Ashwagandha root in reducing stress and anxiety in adults." Indian Journal of Psychological Medicine, 34(3), 255-262. [Indian Journal of Psychological Medicine].
Singh, N., Bhalla, M., de Jager, P., & Gilca, M. (2011). "An overview on Ashwagandha: A Rasayana (rejuvenator) of Ayurveda." African Journal of Traditional, Complementary and Alternative Medicines, 8(5 Suppl), 208-213. [AJTCAM].
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Estrogen: The Essential Hormone for Women’s Health from Puberty to Post-Menopause
Estrogen: The Essential Hormone for Women’s Health from Puberty to Post-Menopause
Estrogen is a hormone that plays a crucial role in a woman’s body from puberty through menopause. It’s often thought of as the "female hormone" because of its importance in female reproduction and overall health, but estrogen also influences nearly every system in the body—from the brain and skin to the heart and bones. Understanding how estrogen works, its different types, and how to monitor it can help women make informed decisions about their hormonal health, especially during the significant transitions of perimenopause and menopause.
The Different Types of Estrogen
There are three main types of estrogen:
Estradiol (E2): The most potent and the primary estrogen produced during reproductive years. Estradiol is essential for ovulation, regulating menstrual cycles, and overall fertility.
Estrone (E1): Predominantly produced after menopause. It is a weaker form of estrogen compared to estradiol and is stored in fat tissue.
Estriol (E3): Known as the weakest estrogen, estriol rises during pregnancy and plays an important role in fetal development. Post-pregnancy, its levels drop significantly.
Among these, estradiol is the most potent and impactful in terms of reproductive health and vitality. It’s responsible for maintaining healthy skin, bones, and mental health, along with supporting fertility and libido.
Estrogen’s Role in Puberty, Fertility, and Beyond
At puberty, estrogen triggers the development of secondary sexual characteristics—such as breast development, widening of hips, and the onset of menstruation. Throughout a woman’s reproductive years, estrogen continues to regulate the menstrual cycle, maintaining the delicate balance needed for fertility and conception.
As women transition from their reproductive years into perimenopause, estrogen levels begin to fluctuate and decline. This stage is often referred to as “puberty in reverse,” as women experience many of the hormonal shifts they did during puberty, but in the opposite direction. Symptoms like mood swings, hot flashes, irregular periods, and difficulty sleeping may arise. Eventually, menopause occurs when the ovaries cease regular function, and estrogen production dramatically decreases.
During this time, estrogen still plays a crucial role in maintaining bone density, heart health, and cognitive function. Post-menopausal women, with lower estrogen levels, are at higher risk for conditions like osteoporosis, heart disease, and cognitive decline.
Hormone Replacement Therapy (HRT), Bioidentical (BHRT), and cBHRT
Many women seek relief from perimenopausal and menopausal symptoms through hormone replacement therapy (HRT). There are three primary types of hormone therapy:
HRT (Hormone Replacement Therapy): Uses synthetic hormones to replace the estrogen your body is no longer producing.
BHRT (Bioidentical Hormone Replacement Therapy): Uses hormones derived from plant sources that are chemically identical to the ones your body produces. Many women find BHRT to be a more natural option.
cBHRT (Compounded Bioidentical Hormone Replacement Therapy): Personalized hormone therapy mixed in specialized compounding pharmacies, tailored to individual hormonal needs.
Choosing the right hormone therapy can help ease the transition and support health during perimenopause and beyond, but it’s important to work closely with a knowledgeable healthcare practitioner to determine the best course of action based on personal needs and hormone levels.
Monitoring Hormone Levels: When and How to Test
Monitoring hormone levels is essential to making informed decisions about hormone therapy and overall health during perimenopause and post-menopause. There are three main ways to test for hormone levels:
Blood (Serum) Testing: Measures the active hormones in your blood at a specific time, giving an immediate snapshot of hormone levels. While commonly used, it only measures the “free” (active) portion of the hormone and may not show how the body is metabolizing estrogen.
Saliva Testing: Measures the “free” fraction of hormones, often used to gauge adrenal function or stress hormones, but less frequently for estrogen.
Urine Testing (DUTCH Test): Provides a more comprehensive view of hormone metabolites, showing not only your hormone levels but also how your body is breaking down and using those hormones. The DUTCH test offers insights into the pathways estrogen follows in your body and can reveal imbalances in metabolism.
Using both serum and the DUTCH test together can provide a more complete picture. Serum gives a snapshot of current levels, while the DUTCH test shows how your body is processing and metabolizing estrogen over a 24-hour period. This combination is particularly useful for women experiencing symptoms of estrogen dominance or depletion, as it helps guide more personalized hormone therapy.
DNA Life Oestrogen Test: Understanding Your Genetic Blueprint
The DNA Life Oestrogen Test offers valuable insight into how your body handles estrogen on a genetic level. This test looks at specific genetic variations (SNPs) that affect estrogen production, metabolism, and detoxification. It helps to determine whether you have a predisposition to conditions influenced by estrogen, such as breast cancer, endometriosis, or osteoporosis.
By understanding your genetic makeup, you and your healthcare provider can take a proactive approach to managing estrogen levels. For example, certain SNPs may indicate that you metabolize estrogen in a way that creates more harmful by-products, increasing your risk for estrogen-related conditions. In such cases, lifestyle modifications, targeted supplements, or specific hormone therapies can be implemented to support safer estrogen metabolism.
The DNA Life Oestrogen Test looks at:
Estrogen receptor genes to understand how sensitive your body is to estrogen.
Detoxification pathways (like COMT and CYP1B1) to see how well your body eliminates estrogen by-products.
Inflammatory markers to assess how estrogen-related inflammation might impact your overall health.
Final Thoughts: The Vital Role of Estrogen
Estrogen is far more than a reproductive hormone. It is a key player in your health and well-being from puberty through post-menopause. Whether you're entering perimenopause, navigating menopause, or exploring hormone therapy options, understanding your body’s estrogen levels and how they impact your health is critical. Using comprehensive hormone testing, like both serum and the DUTCH test, and even genetic insights from the DNA Life Oestrogen Test, can provide a personalized roadmap to managing your hormonal health.
Fun Fact:
Did you know that estriol, one of the three types of estrogen, skyrockets during pregnancy and is about 1,000 times more abundant than at any other time in a woman’s life? It’s the key hormone that helps the placenta grow and supports the baby's development! After pregnancy, estriol levels drop back down, but for those nine months, it’s the reigning queen of estrogen!
Take Control of Your Hormonal Health Today
If you're struggling with perimenopausal symptoms or concerned about how your hormones are impacting your health, now is the time to take action. With the right testing and guidance, you can create a tailored plan to support your estrogen balance and overall wellness. Reach out to schedule a consultation and start your journey to vibrant health today!
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
How the D.R.E.S.S. Protocol and Functional Labs Restore Balance and Resolve Metabolic Chaos®
How the D.R.E.S.S. Protocol and Functional Labs Restore Balance and Resolve Metabolic Chaos®
As a Traditional Naturopath and Functional Diagnostic Nutrition® (FDN) Practitioner, my approach to wellness revolves around identifying and correcting the root causes of Metabolic Chaos®—the state of imbalance when the body's systems are disrupted by hidden dysfunctions. When I incorporated the FDN methodology into my practice, it became clear that the key to true healing lies in uncovering these hidden stressors and restoring balance through a personalized, comprehensive plan.
Metabolic Chaos® is the only diagnosis we use in FDN because it emphasizes that symptoms are not isolated; they are part of a complex web of dysfunction in the body’s systems. By focusing on healing opportunities within the H.I.D.D.E.N.O. categories—Hormonal, Immune, Digestive, Detoxification, Energy production, Nervous system, and Oxidative stress—we can address multiple root causes that are preventing your body from functioning at its best.
To assess these dysfunctions and develop a targeted plan, we rely on foundational labs like the GI-MAP, Oxford Biomedical MRT, Fluids IQ Metabolic Wellness Profile, Fluids IQ Mucosal Barrier Assessment, and the DUTCH hormone panel, combined with DNA testing from DNA Life. Together, these tools offer a clear picture of your body’s current state and provide us with the roadmap to guide you back to health.
The FDN Foundational Labs and Their Role in Uncovering H.I.D.D.E.N.O. Imbalances
GI-MAP (Gastrointestinal Microbial Assay Plus): This test gives us an in-depth look at your gut health by identifying pathogens such as bacteria, fungi, and parasites, along with imbalances in your beneficial microflora. It also measures markers for inflammation and immune response in the gut, like secretory IgA, providing a direct assessment of your gut's mucosal barrier integrity. If there is dysbiosis, SIBO, or pathogenic overgrowth, this test is essential for restoring immune function, digestion, and microflora balance.
Oxford Biomedical MRT (Mediator Release Test): This test helps identify food sensitivities that contribute to inflammation and gut dysfunction. Knowing which foods are triggering an immune response allows us to reduce systemic inflammation, restore gut integrity, and optimize digestion. By removing inflammatory foods and incorporating gut-healing options, we support immune resilience and address digestive dysfunction.
Fluids IQ Metabolic Wellness Profile: This test assesses oxidative stress and mitochondrial function by measuring markers like 8-OHdG, which reflects DNA damage caused by oxidative stress. Oxidative stress is a major contributor to energy production imbalances, chronic fatigue, and brain fog, and by addressing this, we restore cellular vitality and support anti-oxidation.
Fluids IQ Mucosal Barrier Assessment: This test evaluates the integrity of the gut lining by measuring zonulin levels and other markers associated with gut permeability (commonly known as “leaky gut”). A compromised gut lining can allow toxins and undigested food particles into the bloodstream, leading to systemic inflammation and immune dysregulation. By healing the mucosal barrier, we reduce toxic load, improve digestion, and support liver detoxification.
DUTCH (Dried Urine Test for Comprehensive Hormones): This comprehensive hormone test measures your levels of cortisol, DHEA, and sex hormones, giving us key insights into your HPA axis function and hormonal balance. The DUTCH test also evaluates your cortisol rhythms, which are crucial for understanding how chronic stress is impacting your health. Restoring hormonal balance through this test can improve energy levels, stress response, and overall vitality.
DNA Life Nutrigenetic Testing: These tests provide insights into how your unique genetic makeup affects hormone metabolism, detoxification pathways, immune function, and oxidative stress responses. Understanding your genetic predispositions allows us to craft a personalized plan that addresses not only current dysfunctions but also long-term health risks.
Support Strategies Based on Lab Results
After identifying the specific H.I.D.D.E.N.O. dysfunctions through these labs, we implement tailored support strategies to restore balance and optimize health. Here’s how the FDN methodology works across each category:
Support Hormone Balance (HPA Axis Dysfunction)
Through the DUTCH test, we identify imbalances in cortisol and DHEA, which often manifest as chronic fatigue, poor stress resilience, and hormonal disruptions. To restore balance, we use adaptogens like ashwagandha, stress management techniques, and targeted nutrients based on your hormone profile and genetic predispositions.
Support Immune Function
The GI-MAP and MRT results guide us in addressing dysbiosis, pathogenic overgrowth, and food sensitivities that are compromising your immune system. We use probiotics, prebiotics, and immune-modulating supplements to restore microbial balance and strengthen the mucosal barrier. Additionally, insights from the DNA Health profile help us target genetic predispositions to immune dysfunction.
Restore Microflora and Gut Integrity
By addressing the mucosal barrier and gut permeability through the GI-MAP and Fluids IQ Mucosal Barrier Assessment, we heal the gut lining and restore microbial balance. We use gut-healing nutrients like glutamine, aloe vera, and bone broth, and eliminate inflammatory foods identified by the MRT test to promote long-term gut health.
Support Digestion and Assimilation
Maldigestion and malabsorption are common issues uncovered by the GI-MAP and MRT. By introducing digestive enzymes, probiotics, and dietary adjustments, we improve nutrient absorption and optimize digestion, ensuring your body gets the fuel it needs to heal and thrive.
Support Liver Detoxification
A congested liver and poor detoxification can lead to toxin buildup, hormonal imbalances, and oxidative stress. The Fluids IQ Metabolic Wellness Profile helps us assess your detox capacity, while the DNA Detox profile provides genetic insights into how your body processes toxins. We support detox pathways through liver-boosting nutrients like NAC, milk thistle, and dietary strategies that promote efficient toxin elimination.
Support Anti-Oxidation and Energy Production
Through the Fluids IQ Metabolic Wellness Profile, we assess oxidative stress and mitochondrial function. We use antioxidants like CoQ10, alpha-lipoic acid, and other nutrients that support mitochondrial health to reduce oxidative stress, increase energy production, and combat fatigue.
Support Pathogen Eradication
When pathogens are identified through the GI-MAP, we use natural antimicrobial herbs like oregano oil, garlic, and berberine to eradicate harmful bacteria, fungi, or parasites. This helps restore microbial balance and prevent recurring infections or gut dysfunction.
The D.R.E.S.S. Protocol: A Balanced, Root Cause Approach
In our practice, we emphasize the D.R.E.S.S. protocol—Diet, Rest, Exercise, Stress reduction—first because these foundational lifestyle factors are the key to long-term wellness. The last "S" (Supplementation) is introduced later, only after foundational habits are in place, to maximize results and prevent dependency on supplements alone. Here’s how it all comes together:
Diet: Your diet is customized based on lab findings and DNA testing, focusing on anti-inflammatory, whole foods. We prioritize gut-healing foods like prebiotics and fermented foods to support gut health and immune function, while eliminating any foods that exacerbate inflammation or sensitivities.
Rest: Personalized sleep hygiene protocols help to balance cortisol rhythms and support neurotransmitter health. Depending on your DUTCH test results and genetic insights from DNA Mind, we might introduce magnesium, melatonin, or adaptogens to improve your sleep quality.
Exercise: Your exercise plan is aligned with your metabolic and genetic needs. For instance, if we uncover oxidative stress or mitochondrial dysfunction through Fluids IQ testing, we’ll recommend restorative exercises like walking, stretching, and strength training over high-intensity workouts, which could exacerbate fatigue.
Stress Reduction: Stress is often the catalyst for Metabolic Chaos®. Based on DUTCH cortisol results and DNA Mind test outcomes, we incorporate stress management techniques like mindfulness, breathwork, or meditation. If necessary, adaptogenic herbs like ashwagandha or phosphatidylserine will be introduced to help recalibrate your stress response and support the HPA axis.
Supplementation: Once we’ve established a strong foundation through diet, rest, exercise, and stress reduction, we introduce supplements. These will be specifically chosen based on your lab results, such as digestive enzymes for improved digestion, NAC for liver detoxification, or antioxidants like CoQ10 to combat oxidative stress.
Fun Fact:
FDN is the only health coaching program that focuses on identifying Metabolic Chaos®—a state where multiple dysfunctions in the body accumulate and cause symptoms—rather than diagnosing specific conditions. By addressing the root causes through functional lab testing, FDN practitioners aim to "coach up" overall vitality, rather than simply treating or managing disease symptoms!
How I Use the D.R.E.S.S. Protocol in My Practice
By combining the D.R.E.S.S. protocol with functional lab testing and nutrigenetics, I take a holistic, science-driven approach to resolving Metabolic Chaos®. This integrated methodology allows me to tailor each element of the protocol—Diet, Rest, Exercise, Stress reduction, and Supplementation—to your unique biology. Rather than merely managing symptoms, this approach targets the root causes of dysfunction at every level of the body.
To better illustrate how this process works in practice, let’s consider a hypothetical case study.
Case Study: Emily, a 42-Year-Old Executive Struggling with Fatigue and Weight Gain
Emily, a 42-year-old executive, comes to my practice with several complaints: chronic fatigue, unexplained weight gain, digestive discomfort, and difficulty sleeping. She’s also noticed increased irritability and brain fog, which has started affecting her work performance and personal relationships.
After a thorough intake and assessment, it becomes clear that Emily’s lifestyle is high-stress, involving long work hours, poor sleep quality, and inconsistent meal patterns. Despite trying several diets and exercise routines, nothing seems to work, and her symptoms persist.
Given her presentation, I suggest running a set of foundational functional labs to get to the root of her Metabolic Chaos®. We order the GI-MAP, DUTCH test, Fluids IQ Metabolic Wellness Profile, and the Oxford Biomedical MRT test, and we also conduct DNA Life Nutrigenetic Testing to assess her genetic predispositions for hormone metabolism, detoxification, and oxidative stress.
Lab Results and Interpretation
GI-MAP Results: Emily’s test reveals an overgrowth of harmful bacteria, low beneficial gut flora, and elevated markers of gut inflammation, pointing to dysbiosis and leaky gut syndrome. These imbalances are contributing to her chronic fatigue, digestive discomfort, and weakened immune function.
DUTCH Test: Her cortisol levels are dysregulated, showing a flat rhythm in the afternoon and evening, which explains her low energy and difficulty winding down at night. Additionally, her estrogen and progesterone levels are imbalanced, contributing to her mood swings and weight gain around her midsection—typical signs of HPA axis dysfunction.
Fluids IQ Metabolic Wellness Profile: The markers for oxidative stress are elevated, suggesting that Emily’s mitochondria (the energy producers in her cells) are under pressure. This oxidative damage is likely contributing to her fatigue, brain fog, and poor recovery after exercise.
Oxford Biomedical MRT: This test identifies several food sensitivities, including gluten and dairy, which are contributing to systemic inflammation and further exacerbating her gut issues. Removing these trigger foods will be essential for reducing inflammation and healing the gut.
DNA Life Nutrigenetics Testing: Emily’s genetic profile reveals that she has a predisposition to sluggish detoxification and impaired estrogen metabolism. These genetic tendencies have likely worsened her hormone imbalance, making it more difficult for her body to clear excess estrogen and toxins.
Applying the D.R.E.S.S. Protocol
With this detailed information, we craft a personalized D.R.E.S.S. protocol to address the root causes of Emily’s Metabolic Chaos®:
Diet
Based on the MRT and GI-MAP findings, we eliminate gluten, dairy, and other inflammatory foods while introducing gut-healing foods such as fiber rich foods, fermented vegetables, and anti-inflammatory plant foods. I also include specific recommendations from her DNA Life Diet Profile to ensure that her genetic predispositions to nutrient absorption and metabolism are taken into account. This tailored approach not only improves digestion but also supports hormone balance and reduces inflammation.
Rest
The DUTCH test shows that Emily's cortisol levels are out of sync with the natural circadian rhythm, so we implement a customized sleep hygiene routine. This includes mindfulness practices, reducing screen time before bed, and targeted supplements like magnesium and phosphatidylserine to promote relaxation and restore her HPA axis function. By optimizing her sleep and rest, we can enhance her body's ability to repair and regenerate.
Exercise
Emily has been doing high-intensity workouts in an effort to lose weight, but these sessions have been exhausting her. Based on her Fluids IQ Metabolic Wellness Profile, which revealed oxidative stress and mitochondrial dysfunction, we shift her exercise routine to more restorative activities like stretches, walking, and light strength training. This helps her maintain physical activity without further draining her energy reserves, allowing her mitochondria to recover and boosting her stamina over time.
Stress Reduction
The DUTCH test also highlighted the need to regulate her stress response. In addition to mindfulness practices, we introduce adaptogens like ashwagandha and Rhodiola, which support HPA axis recovery. These natural herbs help balance cortisol levels and improve her resilience to stress, both physically and mentally.
Supplementation
Finally, based on Emily’s lab results, we design a targeted supplementation plan:
Probiotics and prebiotics to restore her gut flora based on the GI-MAP.
Digestive enzymes to improve nutrient absorption and ease her digestive discomfort.
Milk thistle and NAC to support liver detoxification, as her genetic testing showed slow detox pathways.
Antioxidants like CoQ10 and alpha-lipoic acid to reduce oxidative stress and support mitochondrial function, improving energy levels.
Magnesium and melatonin to regulate sleep patterns and help restore a healthy circadian rhythm.
Results After 3 Months
After following the D.R.E.S.S. protocol for three months, Emily notices significant improvements. Her energy levels have rebounded, allowing her to perform better at work without the mid-afternoon crashes she once experienced. Her sleep quality has improved, leading to more restorative rest, and her digestion is now smooth and regular, without the discomfort she used to feel after meals.
In terms of weight, Emily has lost the stubborn pounds around her midsection, thanks to her improved hormone balance and reduced inflammation. Most importantly, she feels more in control of her stress levels and mental well-being, and her brain fog has cleared up, allowing her to think and focus more clearly.
The Power of Combining Functional Labs with the D.R.E.S.S. Protocol
Emily’s case illustrates how the D.R.E.S.S. protocol, combined with functional lab testing and nutrigenetic insights, can bring the body back into balance. By targeting her individual needs in each area—diet, rest, exercise, stress reduction, and supplementation—we were able to correct her underlying dysfunctions rather than simply treating her symptoms.
This comprehensive and personalized approach is what sets FDN apart. We don’t guess at what your body needs; we test and use real data to craft a plan that works with your unique biology, ensuring sustainable results and a return to vibrant health.
Conclusion
Achieving true wellness means addressing the root causes of your health issues—not just managing symptoms. Through the use of advanced FDN lab testing and DNA-based insights, we uncover the hidden stressors creating Metabolic Chaos® in your body. The D.R.E.S.S. protocol allows us to systematically coach up vitality and restore balance by focusing on lifestyle factors first, with supplementation used as a final step to optimize your progress.
If you’re ready to move beyond symptoms and get to the root cause of your health challenges, I’m here to help. Together, we’ll create a personalized, holistic plan that will restore your vitality and bring your body back into balance. Contact me today to begin your journey toward optimal health and regain the energy and well-being you deserve!
Citations:
Functional Diagnostic Nutrition. (n.d.). Retrieved from https://www.functionaldiagnosticnutrition.com
GI-MAP: Comprehensive Stool Analysis. Diagnostic Solutions Lab. Retrieved from https://www.diagnosticsolutionslab.com
Nutrigenetics and Genetic Variants: Exploring the Role of Nutrition and Genes. Nutrigenomix. Retrieved from https://www.nutrigenomix.com
Adrenal Stress Profile: Cortisol and DHEA-S Testing. Genova Diagnostics. Retrieved from https://www.gdx.net
Metabolic Chaos and FDN. (n.d.). Retrieved from https://www.functionaldiagnosticnutrition.com
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Implementing the A NEW START Model: A Holistic Approach as a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner
Implementing the A NEW START Model: A Holistic Approach as a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner
When I first became a Traditional Naturopath, I sought to empower individuals with natural healing principles. As part of my practice, I embraced the A NEW START framework—a comprehensive lifestyle model that emphasizes the importance of balance and natural living. Over the years, this model has been a cornerstone of my approach to holistic health, helping clients transform their lives by addressing the root causes of health concerns through diet, exercise, and mindful living.
After becoming a Functional Diagnostic Nutrition® Practitioner (FDN-P), I realized the synergy between functional diagnostic methods and the A NEW START framework. While functional diagnostics allow for deeper insight into physiological imbalances through lab work, A NEW START continues to provide the foundation for a vibrant and healthy life.
Let’s take a closer look at the science and methodology behind the A NEW START framework and how it can support long-lasting vitality.
Attitude: The Power of a Positive Mindset
A positive attitude and mindset is essential for healing. Research shows that stress and negative thinking can impact immune function and hormonal balance. Conversely, a positive attitude can help manage stress levels, improve mood, and foster emotional resilience.
Scientific Support: Studies indicate that optimism and positivity reduce stress hormone levels, lower inflammation, and improve overall health.
Practical Application: Cultivating a positive mindset through gratitude journaling or mindfulness exercises helps reset the nervous system and reduce chronic stress. Incorporating these into your daily routine can significantly enhance your emotional well-being.
Nutrition: Healing Through Food
Nutrition is the cornerstone of health, and the choices we make regarding food directly impact every aspect of our physiology. A nutrient-dense, anti-inflammatory diet full of whole, minimally processed foods provides essential vitamins, minerals, and antioxidants. Minimizing the intake of ultra-processed foods, which are often high in additives and harmful fats, is crucial for reducing inflammation and promoting longevity.
Scientific Support: Research consistently demonstrates that diets rich in fruits, vegetables, and whole grains reduce the risk of chronic diseases like heart disease and diabetes.
Practical Application: I recommend a plant-based, whole-food diet that includes plenty of fiber, healthy fats, and lean proteins. Reducing the intake of processed foods and incorporating natural ingredients into daily meals can dramatically improve digestion, balance hormones, and enhance energy levels.
Exercise: Movement is Medicine
Exercise is critical for physical and mental well-being. Regular movement supports cardiovascular health, improves circulation, and helps regulate hormones. It’s essential to incorporate different types of exercise to address mobility, strength, and endurance.
Scientific Support: Physical activity has been shown to reduce the risk of chronic diseases, boost mood, and improve cognitive function.
Practical Application: Include a variety of exercises in your routine, such as walking, high-intensity interval training (HIIT), stretching, mobility exercises, and strength training. Functional exercises that mimic everyday movements can enhance both strength and flexibility. These activities not only improve physical health such as cardiovascular health but also reduce stress and improve mental clarity.
Water: Hydration for Optimal Health
Water is fundamental to nearly every bodily function, from digestion to detoxification. Drinking clean, filtered water is essential, as many municipal water supplies contain chemicals like fluoride and chlorine, which may have harmful effects on health.
Scientific Support: Hydration is linked to improved cognitive performance and reduced oxidative stress.
Practical Application: Drink filtered or spring water to avoid chemicals like fluoride, chlorine, and other contaminants. Aim to consume at least 8 cups of water a day. Starting the day with a glass of water infused with lemon can enhance hydration and digestion. Proper hydration supports brain function and reduces oxidative stress.
Sunlight: The Healing Power of the Sun
Sunlight is essential for the body’s production of Vitamin D, which supports immune function, hormone regulation, and mood balance. However, how much direct sunlight a person needs varies depending on their skin’s melanin content. Melanin acts as a natural sunscreen, meaning those with darker skin tones (more melanin) require more sunlight exposure to produce the same amount of Vitamin D as those with lighter skin.
Scientific Support: Individuals with lighter skin tones need about 10 to 30 minutes of direct sunlight a few times a week, depending on factors like latitude and time of day.
Those with darker skin tones, who have more melanin, may require 30 minutes to 3 hours of sun exposure to produce adequate Vitamin D. This is due to melanin's ability to filter UVB rays, slowing Vitamin D synthesis.
Practical Application: If you have a darker skin tone and live in a region with limited sunlight, you may need to spend more time outdoors in direct sunlight to achieve optimal Vitamin D levels. Additionally, for those who struggle to get enough natural sunlight—whether due to climate or skin tone—light therapy using devices like full-spectrum or infrared lamps can serve as an alternative. These devices are especially useful during winter months or for individuals living in higher latitudes where sunlight is scarce.
Research shows that adequate sunlight or alternative light exposure helps improve mood, prevent seasonal affective disorder (SAD), and support bone health.
Temperance: Moderation is Key
Practicing temperance involves using good things wisely and avoiding harmful substances, such as alcohol, caffeine, and ultra-processed foods. Regular consumption of these substances can negatively impact metabolic processes and overall health.
Scientific Support: Research highlights the detrimental effects of regular alcohol consumption and processed foods on liver health, metabolism, and cognitive function.
Practical Application: Avoid regular alcohol consumption, reduce reliance on caffeine, and limit processed foods. Practicing temperance promotes balance in both body and mind, allowing for better decision-making and healthier habits.
Air: Breathing in Vitality
Clean air is essential for optimal health, supporting cellular respiration and detoxification. For those living in areas with poor air quality, it’s important to implement strategies that reduce indoor pollutants.
Scientific Support: Poor air quality has been linked to respiratory issues, inflammation, and cardiovascular problems.
Practical Application: If you live in an area with poor air quality, invest in an air purifier and add houseplants like snake plants or spider plants to your home to naturally filter the air. Halotherapy, or salt therapy, can also support respiratory health by helping clear the lungs.
Rest: The Healing Power of Sleep
Restorative sleep is when the body repairs tissues, balances hormones, and restores energy. Sleep deprivation can lead to chronic fatigue, cognitive issues, and increased stress. Observing a day of rest, such as the seventh-day Sabbath, allows for both physical and spiritual rejuvenation.
Scientific Support: Studies show that adequate sleep enhances immune function, regulates mood, and improves cognitive performance.
Practical Application: Establish a consistent sleep routine and ensure your sleep environment is conducive to rest—quiet, dark, and free from distractions. Observing the seventh-day Sabbath allows the body and mind to rest fully and can have a profound effect on overall well-being.
Trust in God: Spiritual Wellness as a Foundation for Health
Trust in the God of the Bible is a vital part of overall well-being. Spiritual health provides strength, peace, and purpose, which can reduce emotional stress and enhance resilience. Proverbs 3:5-6 reminds us to “Trust in the Lord with all your heart and lean not on your own understanding; in all your ways submit to Him, and He will make your paths straight.”
Scientific Support: Numerous studies link spiritual practices such as prayer and faith to improved mental health, emotional resilience, and even longevity.
Practical Application: Regular prayer, meditation, and Bible study offer a sense of peace and trust in God's plan, reducing stress and improving mental health. Incorporating faith into daily life is a cornerstone of overall health.
Fun Fact:
The A NEW START acronym was first developed by the Weimar Institute as part of their lifestyle program, and it's based on natural health principles found in the Bible! Each component is designed to help people live longer, healthier lives by emphasizing whole foods, fresh air, and even faith.
Interestingly, over 11,000 people have participated in Weimar’s residential program, and many have experienced significant improvements in conditions like obesity, diabetes, and hypertension.
How I Apply the A NEW START Model in My Practice
Implementing the A NEW START principles has been transformative in both my personal and professional journey. As a Traditional Naturopath and FDN-P, I’ve seen firsthand how this simple yet powerful framework can empower individuals to take control of their health and live vibrant, fulfilling lives. By integrating the A NEW START methodology with personalized functional diagnostic strategies, you can experience lasting wellness and vitality.
Call to Action: Ready to take the first step towards a healthier, more balanced life? Contact me today for a consultation, and let’s work together to create a personalized plan that aligns with the A NEW START principles. Whether you’re seeking improved energy, better sleep, or overall health, this framework can help you achieve your wellness goals.
References:
Abundant Peace & Health, Principles for Healthy Living
Adventist News Network, NEWSTART Global Health Program
White Throne Ministries, Introduction to NEWSTART
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Exploring the Future of Personalized Medicine: Nutrigenetics and Nutrigenomics
Exploring the Future of Personalized Medicine: Nutrigenetics and Nutrigenomics with DNAlife Genetic Testing
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, my mission is to help you achieve optimal health by uncovering and addressing the root causes of your wellness concerns. In today’s world, where health challenges are often complex and multifaceted, I believe in using the most advanced tools available to provide you with truly personalized care. That’s why I’ve integrated DNAlife genetic testing along with comprehensive functional lab testing into my practice.
DNAlife genetic testing allows us to delve into the unique genetic blueprint that influences how your body responds to the world around you. Through the sciences of nutrigenomics and nutrigenetics, we can explore how your genes affect your response to different nutrients and how your diet and lifestyle choices can impact your gene expression. This knowledge empowers us to create highly customized health plans that cater specifically to your genetic makeup, helping you make informed choices that align with your body’s needs.
But understanding your genetics is just one piece of the puzzle. To get a complete picture of your health, I also rely on functional lab testing, such as the DUTCH test, GI Map, and food sensitivity panels. The DUTCH test provides a detailed analysis of your hormone levels and adrenal health, revealing imbalances that could be affecting your energy, mood, and overall well-being. The GI Map helps us assess the health of your gut microbiome, identifying issues like dysbiosis, infections, or inflammation that might be contributing to digestive discomfort or other systemic issues. Meanwhile, food sensitivity testing allows us to pinpoint foods that could be triggering inflammation or other adverse reactions in your body.
By combining the insights from DNAlife genetic testing with the data from functional lab tests, we can create a comprehensive, personalized plan that addresses your health concerns from every angle. Whether you’re dealing with chronic fatigue, digestive issues, hormonal imbalances, or simply want to optimize your health, this integrative approach ensures we’re not just treating symptoms, but truly supporting your body’s natural ability to heal and thrive.
In this blog, I’ll share more about how DNAlife genetic testing and functional lab tests work together to provide a deeper understanding of your health and how this powerful combination can help you on your journey to vibrant wellness.
Fun Fact
“We are all unique. Our health is determined by our inherent differences combined with our lifestyles and environment. By combining and analysing information about our genome, with other clinical and diagnostic information, patterns can be identified that can help to determine our individual risk of developing disease; detect illness earlier; and, determine the most effective interventions to help improve our health, be they medicines, lifestyle choices, or even simple changes in diet.” -NHS
Understanding Nutrigenetics and Nutrigenomics
Nutrigenetics studies how individual genetic differences affect a person's response to nutrients. Essentially, it looks at how our genes influence the way our bodies metabolize and utilize food. For example, variations in the MTHFR gene can affect how well our bodies process folate, an essential B vitamin. People with certain variations may need more folate in their diet or may benefit from supplementation with methylated forms of the vitamin.
Nutrigenomics, on the other hand, is concerned with how nutrients and dietary components affect gene expression. This means that the food we eat can influence which genes are turned on or off, potentially impacting everything from inflammation levels to our risk of chronic diseases.
These two fields offer profound insights into how we can optimize our health by aligning our diet and lifestyle with our genetic makeup.
What Nutrigenomics and Nutrigenetics Are NOT:
1. One-Size-Fits-All Diet Plans:
Nutrigenomics and nutrigenetics are not about creating universal diet recommendations. These fields recognize that each person has unique genetic variations, known as alleles, which influence how we process and respond to different nutrients. What works for one person, due to their specific alleles, might not be effective for someone else. This means there's no single "best" diet for everyone; rather, diet plans should be personalized to fit your genetic profile.
2. A Magic Bullet for Weight Loss:
Understanding your genetic makeup through nutrigenomics and nutrigenetics can offer insights into how your body responds to certain foods and exercise, but it’s not a guaranteed quick fix for weight loss. These sciences reveal tendencies and preferences based on your alleles—such as how you metabolize fats or carbs—but achieving and maintaining a healthy weight still requires a balanced diet, regular physical activity, and other healthy lifestyle choices.
3. Deterministic or Predictive of Disease:
Nutrigenomics and nutrigenetics do not provide a crystal ball for your health. While they can indicate a predisposition to certain conditions based on your alleles—such as a higher risk of heart disease or diabetes—they do not determine your fate. Your lifestyle, environment, and other factors play significant roles in your overall health. Just because you have a certain allele doesn’t mean you will definitely develop a specific condition; it simply highlights areas where you may need to be more proactive with your health choices.
4. A Replacement for Professional Medical Advice:
These genetic tests provide valuable information, but they are not substitutes for professional medical advice, diagnosis, or treatment. For example, identifying an allele that affects vitamin D metabolism might suggest you need more of this nutrient, but a healthcare provider can help interpret this information in the context of your overall health. Nutrigenomics and nutrigenetics should be part of a broader health strategy that includes regular check-ups and consultations with healthcare professionals.
5. A Diagnostic Tool for Current Health Conditions:
Nutrigenomics and nutrigenetics do not diagnose existing health issues. These tests analyze your alleles to predict how your body might react to different nutrients and lifestyle factors. For instance, if you have an allele that affects how you metabolize caffeine, this insight can help you adjust your intake, but it doesn’t diagnose conditions like insomnia or high blood pressure. Instead, these sciences help you make informed decisions to potentially prevent future health problems, rather than identifying current issues.
DNAlife Genetic Testing: A Comprehensive Approach to Personalized Health
DNAlife offers a comprehensive suite of genetic tests that provide insights into various aspects of health and wellness. Each test is designed to help understand how your genetic makeup influences your body’s response to nutrition, lifestyle, and environmental factors. Here’s an overview of the different DNAlife tests and how they can be beneficial for clients:
The Different DNAlife Tests
DNA Diet
Overview:
The DNA Diet test analyzes genes associated with metabolism, eating behaviors, and how your body responds to different types of fats and carbohydrates. It provides insights into your predisposition for weight gain and how effectively you metabolize different macronutrients.
Benefits:
This test helps in crafting a personalized nutrition plan tailored to your genetic makeup. It can be particularly beneficial for those struggling with weight management, helping them understand whether they may benefit more from a low-carb, low-fat, or Mediterranean-type diet. By knowing your genetic predispositions, you can make informed dietary choices that align with your body's unique needs, potentially improving weight management and overall health.
DNA Health
Overview:
The DNA Health test evaluates genetic variations that influence your overall health and susceptibility to chronic diseases. It covers genes involved in various bodily functions such as detoxification, inflammation, lipid metabolism, bone health, and vitamin metabolism.
Benefits:
This test helps identify potential genetic risks for conditions like heart disease, osteoporosis, and metabolic disorders. By understanding your genetic predispositions, you can take proactive steps to optimize your health, such as adjusting your diet, supplementing with specific nutrients, or implementing lifestyle changes that target areas of genetic vulnerability.
DNA Sport
Overview:
The DNA Sport test focuses on genes related to athletic performance, injury risk, and recovery. It examines genetic variations that affect muscle composition, inflammation, oxidative stress, and cardiovascular capacity.
Benefits:
For athletes and fitness enthusiasts, this test provides insights into the types of physical activities that may be most beneficial for their body. It can guide training and recovery strategies, help prevent injuries, and enhance overall athletic performance by tailoring fitness programs based on genetic strengths and weaknesses.
DNA Mind
Overview:
The DNA Mind test explores genes associated with mental health, cognitive function, and neurodegenerative risk. It covers neurotransmitter pathways, neuroinflammation, and neuroprotection, providing a genetic perspective on mental wellness.
Benefits:
This test is valuable for individuals looking to optimize mental health or those with a family history of cognitive decline. It can help in understanding genetic predispositions to conditions like anxiety, depression, or Alzheimer’s disease, allowing for personalized interventions that promote brain health, such as tailored nutrition, supplementation, and stress management techniques.
DNA Oestrogen
Overview:
The DNA Oestrogen test examines genes involved in estrogen metabolism, which can affect hormone-related health issues. It looks at the pathways for estrogen production, detoxification, and the balance between protective and harmful estrogen metabolites.
Benefits:
This test is particularly beneficial for women concerned about hormone-related conditions such as breast cancer, endometriosis, or menopausal symptoms. It provides insights into how efficiently your body processes estrogen and can guide strategies to optimize hormone balance, such as dietary changes, supplementation, or lifestyle adjustments to support healthy estrogen metabolism.
DNA Resilience
Overview:
The DNA Resilience test focuses on genes related to stress response, anxiety, and mood regulation. It explores how your body handles stress at a genetic level and identifies potential risks for stress-related conditions.
Benefits:
Understanding your genetic resilience to stress can help you develop more effective stress management strategies. This test can guide personalized approaches to mental health, such as tailored relaxation techniques, mindfulness practices, and nutritional support to enhance your body's ability to cope with stress.
DNA Skin
Overview:
The DNA Skin test evaluates genes involved in skin health, including collagen formation, antioxidant protection, pigmentation, and sensitivity to environmental factors like UV radiation.
Benefits:
This test can help tailor skincare routines to your genetic profile, addressing specific concerns such as premature aging, pigmentation issues, or sensitivity. It provides insights into which nutrients and skincare products might be most effective for maintaining healthy, youthful skin based on your genetic predispositions.
The Power of Combining Genetic Testing with Functional Testing
While genetic testing provides valuable insights into your predispositions, combining it with functional testing can offer a more complete picture of your current health. Functional tests assess how well your body is functioning in real-time. This includes hormone levels, gut health, micronutrient status, and more.
Consider a scenario where a client is struggling with chronic fatigue. A DNA Health test may reveal a predisposition to poor mitochondrial function, while functional testing might show a deficiency in CoQ10, a nutrient crucial for energy production. Together, these insights allow for a targeted approach, addressing both the genetic and biochemical contributors to the client's fatigue.
Similarly, someone with a genetic predisposition to insulin resistance revealed through the DNA Diet test can benefit from functional testing that measures current blood glucose levels, insulin sensitivity, and inflammation markers. This combined approach helps in creating a diet and lifestyle plan that is not only preventive but also corrective, targeting the root causes of the client’s symptoms.
Scientific Data Supporting Nutrigenetics and Nutrigenomics
The science behind nutrigenetics and nutrigenomics is rapidly evolving, with numerous studies highlighting their potential. For example, research published in The American Journal of Clinical Nutrition has shown that specific dietary interventions can modulate the expression of genes related to inflammation and oxidative stress, offering a pathway to reducing the risk of chronic diseases .
Moreover, a study in Nature Reviews Genetics outlines how understanding individual genetic variations can lead to more effective dietary recommendations, particularly in managing conditions like obesity and type 2 diabetes .
Putting the Pieces Together: The Jigsaw Puzzle of Health
Think of your health as a jigsaw puzzle, with each piece representing a different aspect—genetics, nutrition, lifestyle, environment, and current health status. By integrating genetic testing with functional diagnostics, we can assemble these pieces to form a complete picture, allowing us to see not just where things might go wrong, but also how to optimize every aspect of your health.
This holistic approach is what sets personalized medicine apart. It's about seeing you as a unique individual with unique needs, rather than applying a cookie-cutter solution to complex health issues.
Conclusion: Take the Next Step Towards Personalized Health
As we continue to explore the possibilities of personalized medicine, the integration of nutrigenetics, nutrigenomics, and functional testing stands out as a revolutionary approach. It provides a deeper understanding of your body and offers actionable insights that can transform your health and well-being.
If you're ready to take control of your health and uncover the unique blueprint that makes you who you are, consider exploring DNAlife genetic testing. Together, we can create a personalized health plan that addresses your specific needs, helps you reach your wellness goals, and ultimately leads to a healthier, happier life.
Contact us today to learn more about how DNAlife testing and functional testing can work for you. Let’s start putting the pieces of your health puzzle together!
Why my practice uses DNAlife
At Leaves from the Tree of Life LLC, we are committed to providing our clients with the most effective and personalized health solutions. We use DNAlife genetic testing because it aligns with our philosophy of treating each individual as unique. DNAlife offers a comprehensive suite of tests that delve into the nuances of your genetic makeup, providing insights that are critical for tailoring personalized nutrition, lifestyle, and wellness plans.
We choose DNAlife because of its scientific rigor and the actionable insights it provides. The tests are backed by extensive research and offer practical, easy-to-understand results that empower our clients to take control of their health. By combining DNAlife genetic testing with our functional diagnostic approaches, we can get to the root causes of health issues, creating customized strategies that address both genetic predispositions and current health status. This integrative approach ensures that our clients receive the most precise, targeted care, helping them achieve optimal health and well-being.
Citations:
Nutrigenetics:
1. Study on MTHFR Gene and Folate Metabolism:
- Citation: Bailey, L. B., & Gregory, J. F. (1999). Folate metabolism and requirements. The Journal of Nutrition, 129 (4), 779-782.
- Website: [Folate metabolism and requirements - The Journal of Nutrition]
2. Nutrigenetic Influences on Lipid Metabolism:
- Citation: Corella, D., & Ordovas, J. M. (2009). Nutrigenomics in cardiovascular medicine. Circulation: Cardiovascular Genetics, 2 (6), 637-651.
- Website: [Nutrigenomics in Cardiovascular Medicine - Circulation: Cardiovascular Genetics]
Nutrigenomics:
1. Dietary Impact on Gene Expression:
- Citation: Bishop, K. S., & Ferguson, L. R. (2015). The interaction between epigenetics, nutrition, and the development of cancer. Nutrients, 7 (2), 922-947.
- Website: [The Interaction Between Epigenetics, Nutrition, and the Development of Cancer - Nutrients]
2. Nutrigenomics and Inflammation:
- Citation: Minihane, A. M., & Jofre-Monseny, L. (2007). Impact of genotype on cardiovascular disease risk: a focus on nutrigenetics and nutrigenomics. Public Health Nutrition, 10 (10A), 1253-1260.
- Website: [Impact of Genotype on Cardiovascular Disease Risk - Cambridge University Press]
Personalized Medicine & DNAlife Genetic Testing:
1. Genetic Testing for Personalized Nutrition:
- Citation:
Grimaldi, K. A., van Ommen, B., Ordovas, J. M., Parnell, L. D., Mathers, J. C., & Bendik, I. (2017). Personalized nutrition: paving the way to better population health. The British Medical Journal (BMJ), 361, k2173. doi:10.1136/bmj.k2173.
Website: Personalized nutrition: paving the way to better population health - BMJ
2. DNAlife and Nutrigenetics in Clinical Practice:
- Citation: Fenech, M. (2012). Nutrigenetics and nutrigenomics: viewpoints on the current status and applications in nutrition research and practice. Journal of Nutrigenetics and Nutrigenomics, 5(1), 35-43.
- Website: [Nutrigenetics and Nutrigenomics: Viewpoints on the Current Status and Applications - Karger]
These references and websites provide a comprehensive look at how nutrigenetics and nutrigenomics are being used to advance personalized medicine through genetic testing and personalized nutrition strategies.
Nature Reviews Genetics citation:
Citation:
Zeevi, D., Korem, T., Zmora, N., Israeli, D., Rothschild, D., Weinberger, A., ... & Segal, E. (2015). Personalized nutrition by prediction of glycemic responses. Nature, 518(7538), 512-516. doi:10.1038/nature14202.
Website:
[Personalized nutrition by prediction of glycemic responses - Nature]
This reference provides insights into how personalized nutrition can be developed by understanding individual glycemic responses to food, highlighting the importance of nutrigenomics and nutrigenetics in crafting dietary recommendations based on genetic profiles.
The American Journal of Clinical Nutrition citation:
Citation:
Calder, P. C., Ahluwalia, N., Brouns, F., Buetler, T., Clement, K., Cunningham, K., ... & de Vries, J. H. (2011). Dietary factors and low-grade inflammation in relation to overweight and obesity. The American Journal of Clinical Nutrition, 93(3), 413-420. doi:10.3945/ajcn.110.004777.
Website:
This article explores how various dietary factors can modulate inflammation and how these interactions are influenced by genetic variations. It provides a scientific basis for understanding the role of nutrigenomics in personalized nutrition strategies.
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
The Health Benefits of Fitness, Exercise, and Mobility: A Naturopathic and Functional Approach
The Health Benefits of Fitness, Exercise, and Mobility: A Naturopathic and Functional Approach
Fitness and mobility are essential for maintaining health throughout life, and as we age, they become even more critical. As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I encourage a proactive approach to health, emphasizing the role of exercise in physical, mental, and emotional well-being. In this article, we will explore the diverse benefits of exercise, how to tailor workouts for different body types—including hybrid types—and delve into the best times to exercise based on DNAlife’s Nutrigenomics and Nutrigenetics insights. Additionally, I will highlight the importance of preserving muscle mass as one ages and provide data on the natural decline of muscle with age. I will conclude with a call to action, inviting you to take your fitness to the next level with a complimentary discovery call.
Fun Fact:
Did you know that muscle is one of the most metabolically active tissues in the body, even at rest? This means that having more muscle mass can actually boost your metabolism, helping you burn more calories throughout the day—even when you're just sitting or sleeping! This is why strength training is so effective not just for building strength, but also for long-term weight management and metabolic health. So, as you age, maintaining muscle mass isn't just about staying strong—it's also about keeping your metabolism revved up!
The Health Benefits of Exercise
Physical Health Benefits:
Regular exercise boosts cardiovascular health, strengthens muscles, maintains bone density, and aids in weight management. It also supports the body’s immune function and reduces the risk of chronic diseases like hypertension, diabetes, and arthritis.
Mental and Emotional Well-being:
Exercise releases endorphins, which act as natural mood enhancers, reducing anxiety and depression. It improves sleep quality and cognitive function, making it an excellent tool for managing stress and enhancing overall mental clarity.
Mobility and Flexibility:
Maintaining mobility through flexibility exercises such as dynamic stretching is crucial for preventing injuries and ensuring long-term physical autonomy. Flexibility work promotes joint health and posture while improving coordination and balance.
Different Types of Exercises and Their Benefits
1. Cardiovascular Exercise:
Examples: Running, swimming, cycling, rowing, brisk walking.
Benefits: Cardiovascular exercise strengthens the heart and lungs, improves circulation, boosts stamina, and supports fat loss. It also improves mental health by releasing endorphins, enhances mood, and can help regulate sleep patterns. Regular cardio reduces the risk of chronic conditions such as heart disease, hypertension, and type 2 diabetes.
Additional Benefits: Helps improve endurance and overall energy levels, making daily tasks easier. For those looking to maintain a healthy weight, cardio exercises are effective for burning calories and managing body fat.
2. Strength Training:
Examples: Weightlifting (dumbbells, barbells), resistance bands, bodyweight exercises like push-ups, squats, and pull-ups.
Benefits: Strength training builds muscle mass, enhances bone density, supports joint health, and increases metabolic rate. It also improves muscle tone, supports posture, and helps prevent age-related muscle loss (sarcopenia). Incorporating resistance training into a fitness routine can aid in improving strength, coordination, and stability, making everyday movements more efficient.
Additional Benefits: Strength training boosts metabolism, which can continue burning calories even after a workout. It also reduces the risk of osteoporosis and improves balance, decreasing the likelihood of falls, especially in older adults.
3. Flexibility and Mobility:
Examples: Dynamic stretching, foam rolling, resistance band stretches, joint mobility drills, and functional movement stretches.
Benefits: Flexibility and mobility exercises improve joint range of motion, reduce muscle tension, and support posture. These movements prepare the body for physical activity and help prevent injuries by increasing blood flow to muscles and improving muscle elasticity.
3.1 Examples of Flexibility and Mobility Movements:
Dynamic Lunges with a Twist: Improves hip flexor mobility and spine rotation.
Hip Circles: Increases mobility in the hips, which is essential for squats and lower body movements.
Shoulder Rolls: Helps increase range of motion in the shoulders and prevents stiffness.
Leg Swings: Dynamic leg swings help loosen the hips and hamstrings, preparing them for athletic activity.
Cat-Cow Stretch (without yoga focus): Improves spinal flexibility by moving the back through flexion and extension.
Scapular Wall Slides: Enhances shoulder mobility and strengthens the muscles responsible for proper posture.
Additional Benefits: Flexibility and mobility exercises reduce stiffness, alleviate aches and pains, and improve coordination. This is essential for maintaining independence as we age, allowing for greater freedom of movement and a reduced risk of falls or injuries.
4. High-Intensity Interval Training (HIIT):
Examples: Sprinting, burpees, jump squats, mountain climbers, kettlebell swings, and battle ropes.
Benefits: HIIT involves short bursts of intense exercise followed by periods of rest or lower-intensity activity. It enhances cardiovascular health, increases metabolic rate, and is highly effective for burning calories and fat. HIIT is time-efficient, often requiring only 20-30 minutes per session to achieve significant benefits.
Additional Benefits: HIIT improves both aerobic and anaerobic endurance, making it an ideal choice for those looking to maximize fitness gains in a short time. It also stimulates muscle growth and improves insulin sensitivity, which helps regulate blood sugar levels.
5. Functional Training:
Examples: Squats, lunges, deadlifts, push-ups, kettlebell swings, and farmer’s carries.
Benefits: Functional training focuses on movements that mimic everyday activities, such as lifting, pulling, pushing, and squatting. This type of exercise improves strength, balance, coordination, and flexibility, making daily tasks easier and reducing the risk of injury. It strengthens the core and stabilizer muscles, which are critical for maintaining proper posture and preventing back pain.
Additional Benefits: Functional exercises improve athletic performance by enhancing agility, balance, and coordination. These movements help build a strong foundation, making other types of workouts (e.g., strength training and cardio) more effective. Functional training also improves joint stability, which is essential for longevity in both fitness and daily life.
Understanding Body Types and Exercise: Including Hybrid Body Types
Tailoring workouts to individual body types can maximize results. Alongside the classic body types—ectomorph, mesomorph, and endomorph—many people display traits of hybrid types, combining characteristics from two or more categories.
Understanding Body Types and Hybrid Combinations: Tailoring Your Workout for Optimal Results
Your body type plays a crucial role in how you respond to various forms of exercise and nutrition. While the three classic body types—ectomorph, mesomorph, and endomorph—are foundational, most individuals are a hybrid of two types, with unique characteristics and responses to exercise. Customizing your workout based on your body type, including hybrid variations, can maximize your progress and help achieve your fitness goals more efficiently.
Primary Body Types:
1. Ectomorph:
Characteristics: Naturally lean, with long limbs, and often finds it difficult to gain both muscle and fat.
Recommended Exercise: Ectomorphs should focus on resistance training to build muscle mass. Compound lifts, such as deadlifts, squats, and bench presses, are highly beneficial. Minimize cardio to avoid further fat loss, and prioritize a calorie surplus in your diet to support muscle growth.
2. Mesomorph:
Characteristics: Naturally muscular, well-proportioned, and highly responsive to resistance training. Gains muscle and strength easily.
Recommended Exercise: A balanced routine combining strength training and cardio is ideal. Mesomorphs excel with HIIT (high-intensity interval training) and moderate-weight, high-rep lifting routines. Their ability to recover quickly makes them adaptable to various types of workouts.
3. Endomorph:
Characteristics: Tends to store fat easily, particularly around the midsection, and often struggles with weight loss.
Recommended Exercise: Focus on high-intensity cardio and strength training to build muscle while shedding fat. Circuit training and HIIT are particularly effective for endomorphs, as they burn calories while improving muscular endurance. Consistency and diet management are key to managing weight.
Hybrid Body Types
1. Ecto-Mesomorph (Ectomorph + Mesomorph Traits)
Characteristics: This hybrid body type combines the naturally lean frame of the ectomorph with the muscular potential of the mesomorph. Individuals with these traits tend to be slender but can build muscle more easily than pure ectomorphs. However, they may still find it difficult to gain excess fat, which means they need to focus on a balanced approach to exercise and nutrition to ensure muscle growth without overdoing fat loss.
Recommended Exercise: Ecto-mesomorphs should focus heavily on strength training, particularly hypertrophy-based workouts with moderate weights and higher repetitions. This approach will maximize muscle growth while maintaining the lean look they naturally possess. Incorporating compound movements like squats, deadlifts, and bench presses is key. While cardio isn't the main focus, low to moderate interval-based cardio can be beneficial to improve endurance and maintain cardiovascular health without burning too many calories that are needed for muscle growth.
2. Meso-Endomorph (Mesomorph + Endomorph Traits)
Characteristics: This combination features the muscular build of a mesomorph with the fat-retaining tendency of an endomorph. These individuals typically build muscle easily, but also struggle with fat accumulation, especially in areas like the midsection. Without careful dietary and exercise management, they may experience unwanted fat gain along with their muscle growth.
Recommended Exercise: For meso-endomorphs, the focus should be on fat loss while preserving muscle mass. A combination of high-intensity interval training (HIIT) and strength training will be most effective. Circuit training and functional exercises are ideal for keeping the heart rate up while building muscle. Additionally, incorporating core-focused exercises like planks, Russian twists, and leg raises will help combat fat storage in the midsection. Mesomorphic traits allow them to excel in both endurance and strength-based workouts, making them versatile in their approach.
3. Ecto-Endomorph (Ectomorph + Endomorph Traits)
Characteristics: This body type features a slim upper body, akin to an ectomorph, but with a tendency to store fat in the lower body, especially around the hips, thighs, and sometimes the abdomen. These individuals may find it challenging to balance maintaining a lean upper body while reducing fat in the lower body.
Recommended Exercise: Ecto-endomorphs should focus on full-body strength training with particular emphasis on lower-body resistance exercises such as squats, lunges, and deadlifts to build muscle in the legs and glutes while promoting fat loss. Pairing strength work with steady-state cardio or moderate-intensity interval training will help to burn fat, particularly from the lower body, without sacrificing muscle in the upper body. Including functional lower-body movements like step-ups and kettlebell swings can also enhance results.
4. Endomorphic Mesomorph (Mesomorph + Endomorph)
Characteristics: This hybrid body type has the strength and muscular capacity of a mesomorph with the fat-storing characteristics of an endomorph. Typically, these individuals are naturally muscular but need to be cautious of excess fat gain, especially in areas like the abdomen and thighs.
Recommended Exercise: Endomorphic mesomorphs should adopt a program that focuses on strength training to build and maintain muscle, coupled with high-intensity cardio to stimulate fat burning. Circuit training or HIIT will provide the necessary stimulus for fat loss while keeping muscle intact. Core strengthening exercises such as mountain climbers and ab rollouts should be included to manage midsection fat. Nutritional management is key for this body type to prevent excessive fat gain while building muscle.
5. Ectomorphic Mesomorph (Mesomorph + Ectomorph)
Characteristics: With the lean frame of an ectomorph but the muscle-building potential of a mesomorph, this body type has a natural advantage in achieving a balanced, athletic physique. Ectomorphic mesomorphs can build muscle effectively without gaining much fat, giving them a streamlined, muscular look.
Recommended Exercise: The ideal exercise program for an ectomorphic mesomorph should emphasize moderate-to-heavy weightlifting to enhance muscle size and strength. Since these individuals may not store much fat, their cardio can be limited to low-impact, steady-state activities for cardiovascular health, such as cycling or swimming, ensuring that calorie burn doesn't impede muscle growth. This body type can benefit from a split training routine, focusing on different muscle groups each day to maximize hypertrophy.
6. Mesomorphic Ectomorph (Ectomorph + Mesomorph)
Characteristics: Mesomorphic ectomorphs have a naturally lean, narrow build like an ectomorph, but with the added ability to build muscle like a mesomorph. However, gaining significant mass can still be a challenge, especially if they don’t follow a structured, progressive workout and diet regimen.
Recommended Exercise: Strength training is key for mesomorphic ectomorphs, with a focus on compound movements and progressive overload to promote muscle gain. A higher calorie intake with protein-rich meals will support muscle-building efforts. Incorporating short bursts of cardio, like interval sprints, can help maintain cardiovascular health without limiting muscle growth. Because of their ectomorphic tendencies, rest and recovery are crucial to avoid overtraining and to give muscles time to grow.
7. Endomorphic Ectomorph (Endomorph + Ectomorph)
Characteristics: This combination presents with a slender frame and a slow metabolism, making it challenging to gain muscle without also gaining fat. While these individuals are typically slim, they can gain fat in areas like the lower body or midsection if not careful with diet and exercise.
Recommended Exercise: Endomorphic ectomorphs benefit from a balance of strength training and cardiovascular work. Incorporating moderate-intensity cardio (e.g., cycling or jogging) will help regulate body fat, while full-body resistance exercises will help them build muscle. Since this type may struggle to gain muscle, it’s important to focus on progressive resistance training, ensuring they increase weights and reps over time. Keeping their metabolism active through regular exercise and balanced meals is essential.
Tailoring Your Routine for Maximum Results:
Ectomorphs: Prioritize strength and resistance training, keeping cardio to a minimum to avoid hindering muscle gain.
Mesomorphs: Use a mix of varied strength training and cardio. Mesomorphs can handle a variety of routines, excelling in high-intensity workouts.
Endomorphs: Combine high-intensity cardio with resistance training, focusing on fat loss and muscle maintenance.
For hybrid body types, integrating training methods suited for both components of your hybrid classification will yield the best results.
Best Times to Exercise According to DNAlife’s Nutrigenomics and Nutrigenetics
DNAlife’s Nutrigenomics and Nutrigenetics analyze genetic markers that influence exercise timing for optimal performance and recovery. By personalizing workout schedules based on DNA, you can enhance your fitness outcomes.
DNA Sport
Sample report
1. Morning Workouts:
Ideal for those with early energy peaks. Morning exercise boosts metabolism, improves focus, and sets a positive tone for the day. It’s great for weight loss and maintaining lean muscle mass.
2. Afternoon/Evening Workouts:
Some individuals have a genetic predisposition for peak physical performance in the afternoon or evening. Muscle strength, flexibility, and endurance often peak during this time, making it perfect for strength training or high-intensity workouts.
3. Timing May Not Matter:
For some, the time of day may not impact exercise performance or recovery. Consistency is key, so exercising at a time that fits your schedule is most important.
DNAlife Sport and Personalized Fitness Optimization
DNA Sport
Sample report
DNAlife Sport offers genetic testing that provides insights into how your genes impact athletic performance, recovery, and training. The service helps you tailor workouts to match your genetic makeup for optimal results.
Recovery Optimization: DNAlife Sport identifies how quickly your body recovers from exercise based on genetic markers related to inflammation and muscle repair. This allows for better recovery strategies to avoid overtraining.
Personalized Nutrition: DNAlife Sport also offers insights into how well your body processes nutrients such as vitamins and minerals. For example, genes that affect vitamin D or iron absorption can impact endurance and strength, making nutrition adjustments key.
Injury Prevention: Genetic insights reveal predispositions to specific injuries, such as ligament tears or tendonitis, and help tailor training programs to minimize risks.
The Importance of Fitness, Exercise, and Mobility as We Age
As we age, staying physically active becomes even more crucial for maintaining overall health and well-being. One significant issue to be mindful of is sarcopenia, the age-related loss of muscle mass. Studies show that muscle mass decreases by approximately 3-8% per decade after the age of 30, with the rate of decline increasing after age 60. This decline in muscle mass leads to reduced strength, mobility, and balance, increasing the risk of falls and fractures.
Why Maintaining Muscle Mass is Critical:
Metabolic Health: Muscle mass is metabolically active tissue. As we age, maintaining muscle helps regulate blood sugar levels and improves insulin sensitivity, reducing the risk of type 2 diabetes.
Bone Health: Strong muscles support bone density, reducing the risk of osteoporosis. Muscle contractions during strength training stimulate bone growth, which is especially important for postmenopausal women.
Independence and Mobility: Maintaining muscle strength and joint mobility supports independence as we age. It allows for easier performance of daily tasks such as lifting groceries, climbing stairs, and even getting out of a chair.
Injury Prevention: Muscle acts as a cushion for bones and joints, reducing the risk of injury. It also helps improve balance, which is crucial in preventing falls in older adults.
How Strength Training Helps as You Age
Strength training is one of the most effective ways to combat sarcopenia. Regular resistance exercises, such as lifting weights, using resistance bands, or even bodyweight exercises like push-ups, can help maintain and build muscle mass. Strength training also improves bone density, balance, and coordination, all of which are vital for aging gracefully.
Recommended Strength Exercises for Aging Adults:
1. Bodyweight Exercises: Squats, lunges, and push-ups are excellent for building muscle without the need for equipment.
2. Resistance Bands: Bands provide gentle resistance and are perfect for improving muscle tone without putting strain on joints.
3. Weightlifting: For those able, lifting light to moderate weights 2-3 times a week can significantly slow the loss of muscle mass and promote overall strength and health.
Conclusion
Maintaining fitness, exercise, and mobility as we age is essential for promoting longevity, independence, and quality of life. Whether you’re focusing on building muscle, improving flexibility, or maintaining cardiovascular health, a personalized approach to exercise is key. By leveraging insights from DNAlife’s Nutrigenomics and Nutrigenetics, you can tailor your fitness routine for optimal results. And, as muscle mass naturally declines with age, incorporating strength training into your routine is critical for staying strong and active.
Ready to start or optimize your fitness journey? Book a complimentary discovery call today, and let’s work together to create a personalized plan that fits your unique needs. Together, we’ll help you stay strong, healthy, and mobile for years to come.
Quinoa & Lentil Power Bowl with Tahini Dressing
Here’s a delicious whole food, plant-based recipe that aligns perfectly with the fitness and muscle-maintenance focus of the blog article. This recipe is packed with plant-based protein, fiber, and essential nutrients to support muscle recovery and overall health.
Quinoa & Lentil Power Bowl with Tahini Dressing
Ingredients:
For the Bowl:
1 cup quinoa (rich in protein and fiber)
1 cup cooked lentils (packed with protein and iron)
1 medium sweet potato, diced (high in antioxidants and vitamin A)
1 cup kale, chopped (rich in vitamins C and K)
1/2 cup cherry tomatoes, halved (for vitamin C and antioxidants)
1/4 cup pumpkin seeds (for magnesium, zinc, and healthy fats)
1/2 avocado, sliced (for healthy fats and potassium)
1 tsp olive oil (optional, for roasting sweet potato)
For the Tahini Dressing:
2 tbsp tahini (rich in calcium and healthy fats)
1 tbsp lemon juice (for vitamin C)
1 tsp maple syrup (natural sweetness)
1 garlic clove, minced
2-3 tbsp water (to thin the dressing)
Salt and pepper to taste
Instructions:
1. Cook the Quinoa:
Rinse the quinoa and cook it in 2 cups of water. Bring to a boil, then reduce to a simmer and cook until the water is absorbed (about 15 minutes). Fluff with a fork and set aside.
2. Roast the Sweet Potatoes:
Preheat the oven to 400°F (200°C). Toss the diced sweet potato with olive oil (optional) and roast on a baking sheet for 20-25 minutes or until tender and lightly caramelized.
3. Cook the Lentils:
While the sweet potatoes roast, cook the lentils according to package instructions (about 15-20 minutes), then drain and set aside.
4. Prepare the Vegetables:
Massage the chopped kale with a little lemon juice and salt to soften it.
Slice the avocado and halve the cherry tomatoes.
5. Make the Tahini Dressing:
Whisk together the tahini, lemon juice, maple syrup, minced garlic, water, and a pinch of salt and pepper. Adjust the water to reach your desired consistency.
6. Assemble the Power Bowl:
Divide the quinoa, lentils, and roasted sweet potatoes into bowls. Top with kale, cherry tomatoes, avocado slices, and pumpkin seeds.
Drizzle generously with the tahini dressing.
7. Enjoy:
This bowl is nutrient-dense, providing a balance of protein, complex carbohydrates, healthy fats, and essential vitamins and minerals. It's perfect for muscle recovery and fueling your active lifestyle!
Nutrition Benefits:
Quinoa and lentils are complete proteins, providing all nine essential amino acids needed for muscle repair and maintenance.
Pumpkin seeds add magnesium and zinc, which are crucial for muscle function and recovery.
Sweet potatoes provide complex carbohydrates for sustained energy, making this dish ideal for post-workout recovery.
Enjoy this power-packed, whole food, plant-based meal that supports your fitness goals!
Citations and Resources:
1. Harvard Health Publishing – The Importance of Strength Training as You Age: [https://www.health.harvard.edu/staying-healthy/the-importance-of-strength-training-as-you-age]
2. National Institutes of Health – Muscle Mass Decline with Age: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2804956/]
3. DNAlife – Nutrigenomics & Nutrigenetics Information: [https://www.dnalife.healthcare]
4. National Institute on Aging – Muscle Health and Aging: [https://www.nia.nih.gov/news/strength-training-important-everyone-especially-aging]
5. PubMed – Sarcopenia and Muscle Loss in Older Adults: [https://pubmed.ncbi.nlm.nih.gov/26667010/]
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
The Health Benefits of a Whole Food Plant-Based Diet: A Return to Our Roots
The Health Benefits of a Whole Food Plant-Based Diet: A Return to Our Roots
As a Seventh-day Adventist and a practitioner of Traditional Naturopathy and Functional Diagnostic Nutrition®, I am deeply passionate about how our diet influences our health and overall well-being. Contrary to current interpretations of our ancestors' diets, such as the paleo and other popular diet trends, scientists have discovered that early humans primarily consumed plant-based foods. A whole food plant-based diet not only supports optimal health but also aligns with how our ancestors—especially the first humans described in the Bible—nourished themselves. Let’s explore the profound benefits of this diet and its deep connection to ancient dietary wisdom.
Fun Fact
Genesis 1:29
Then God said, “I now give you every seed-bearing plant on the face of the entire earth and every tree that has fruit with seed in it. They will be yours for food.
A Biblical Perspective on Diet: The First Humans
In the Bible, the diet of the first humans, Adam and Eve, is depicted as plant-based. Genesis 1:29 states, "And God said, 'Behold, I have given you every herb bearing seed, which is upon the face of all the earth, and every tree, in the which is the fruit of a tree yielding seed; to you it shall be for meat.'" This verse suggests that the original diet intended for humans was rich in fruits, vegetables, nuts, and seeds — the foundational elements of a whole food plant-based diet.
This diet is abundant in nutrients, fibres, and natural sugars, providing all the essentials needed for the body to thrive. The simplicity and purity of this diet resonate with many health-conscious individuals today who seek to eat closer to nature.
What is a Whole Food Plant-Based Diet?
A whole food plant-based diet is a way of eating that focuses on consuming unprocessed or minimally processed plant foods in their most natural form. This dietary approach emphasizes the quality and variety of foods, ensuring they are nutrient-dense and derived primarily from plant sources. Unlike some other diets that may permit a wide range of processed and animal-based foods, a whole food plant-based diet prioritizes foods that come directly from nature with minimal alteration.
Here’s a closer look at what constitutes a whole food plant-based diet:
Fruits and Vegetables
Fruits and vegetables form the cornerstone of a whole food plant-based diet. They are packed with essential vitamins, minerals, antioxidants, and phytochemicals that support overall health and wellness. Fresh, frozen, and dried fruits and vegetables are all included, offering a diverse array of flavours and nutrients.
Fruits: Apples, oranges, berries, bananas, mangoes, and more are encouraged. These provide natural sugars, fibre, vitamins, and a host of other nutrients that are crucial for maintaining health.
Vegetables: Both leafy greens (like spinach and kale) and starchy vegetables (like sweet potatoes and squash) are staples. These provide essential nutrients such as vitamins A, C, and K, as well as minerals like potassium and magnesium.
Whole Grains
Whole grains are a key component of a whole food plant-based diet. Unlike refined grains, which have been stripped of their nutrient-rich bran and germ, whole grains retain all parts of the grain kernel, providing a rich source of fibre, protein, and essential nutrients.
Examples of Whole Grains: Brown rice, quinoa, oats, barley, farro, bulgur, and whole wheat. These grains are minimally processed to retain their full nutritional profile and are an excellent source of complex carbohydrates that provide sustained energy.
Legumes
Legumes, which include beans, lentils, chickpeas, and peas, are a fantastic source of plant-based protein. They are also rich in fibre, iron, and folate, making them an essential component of a balanced plant-based diet.
Examples of Legumes: Black beans, kidney beans, lentils, chickpeas, and split peas. These versatile ingredients can be used in soups, stews, salads, and more, providing a hearty texture and a wealth of nutrients.
Nuts and Seeds
Nuts and seeds are nutrient-dense foods that provide healthy fats, protein, and a variety of vitamins and minerals. They are a great addition to a whole food plant-based diet due to their versatility and nutritional benefits.
Examples of Nuts and Seeds: Almonds, walnuts, cashews, flaxseeds, chia seeds, sunflower seeds, and pumpkin seeds. These can be eaten as snacks, blended into smoothies, sprinkled on salads, or used in baking and cooking.
Healthy Fats
While a whole food plant-based diet is low in unhealthy fats, it does include healthy fats that are essential for brain health, hormone production, and overall cell function. These fats come from whole food sources rather than processed oils.
Sources of Healthy Fats: Avocados, olives, nuts, seeds, and coconut. These foods provide monounsaturated and polyunsaturated fats, which are known to support heart health and reduce inflammation.
Minimally Processed Foods
A whole food plant-based diet encourages foods that are as close to their natural state as possible. This means avoiding highly processed foods, refined sugars, and artificial additives that can compromise nutritional quality and contribute to health problems.
Examples of Minimally Processed Foods: Whole grain bread made from 100% whole grains, tofu, tempeh, and plant-based milk alternatives like almond milk or oat milk (preferably unsweetened and without added preservatives).
Herbs and spices are an important part of a whole food plant-based diet, providing not only flavour but also potent antioxidants and anti-inflammatory properties. These natural seasonings can enhance the taste of meals without the need for added salt or unhealthy fats.
Examples of Herbs and Spices: Basil, oregano, turmeric, cinnamon, garlic, ginger, cumin, and coriander. These can be used fresh or dried and are a great way to add depth and nutrition to any dish.
What to Avoid and Limit on a Whole Food Plant-Based Diet
A whole food plant-based (WFPB) diet is centred around consuming minimally processed, nutrient-dense plant foods, while avoiding or limiting foods that are processed, refined, or detrimental to health. Here’s a breakdown of what to avoid or limit to fully reap the benefits of a WFPB lifestyle:
Processed and Refined Foods
What to Avoid: Highly processed foods such as packaged snacks, frozen meals, and processed plant-based alternatives (like mock meats) often contain unhealthy additives, preservatives, and refined ingredients that strip away the natural nutrients of whole foods.
Why: These foods are typically high in sodium, unhealthy fats, and added sugars, contributing to inflammation, weight gain, and an increased risk of chronic diseases like heart disease and diabetes.
What to Choose Instead: Focus on whole, unprocessed foods such as fresh fruits, vegetables, whole grains, legumes, nuts, and seeds.
Refined Grains
What to Avoid: White bread, white rice, pasta made from refined flour, and other refined grains are stripped of their natural fibre, vitamins, and minerals during processing.
Why: Refined grains can cause spikes in blood sugar and offer little nutritional value compared to whole grains.
What to Choose Instead: Opt for whole grains like brown rice, quinoa, barley, oats, and whole wheat products, which provide essential nutrients and sustained energy.
Added Sugars and Sweeteners
What to Avoid: Processed foods often contain added sugars, including high fructose corn syrup, cane sugar, and artificial sweeteners.
Why: Excessive sugar intake can lead to weight gain, insulin resistance, and an increased risk of cardiovascular disease. Artificial sweeteners may also have negative effects on gut health and metabolic function.
What to Choose Instead: Use natural sweeteners sparingly, such as dates, maple syrup, or fruit. Emphasise naturally sweet whole fruits like berries, apples, and bananas.
Oils and Fats
What to Avoid: Refined oils, particularly those high in saturated and trans fats, such as vegetable oil, canola oil, palm oil, and hydrogenated oils.
Why: Oils are highly processed and calorie-dense, often contributing to weight gain, inflammation, and heart disease. Even plant-based oils, while better than animal fats, should be limited.
What to Choose Instead: Obtain healthy fats from whole food sources like avocados, nuts, seeds, and olives, which provide fibre and essential fatty acids without the drawbacks of refined oils.
Animal Products
What to Avoid: Meat, dairy, eggs, and other animal products are typically excluded from a whole food plant-based diet.
Why: Research shows that reducing or eliminating animal products can lower the risk of chronic diseases such as heart disease, cancer, and diabetes. Animal-based foods tend to be high in saturated fat and cholesterol, which can contribute to inflammation and heart disease.
What to Choose Instead: Prioritise plant-based protein sources like beans, lentils, tofu, tempeh, and quinoa, which are not only nutrient-dense but also provide fibre and antioxidants.
Processed Plant-Based Meats and Dairy Alternatives
What to Avoid: While plant-based alternatives like veggie burgers, mock meats, and non-dairy cheeses can be convenient, many are highly processed and contain additives, oils, and sodium.
Why: These processed foods can be less healthy than whole food options, lacking in fibre and containing added ingredients that can diminish their nutritional value.
What to Choose Instead: Make your own plant-based versions using whole ingredients, such as homemade veggie burgers made from beans and grains, or cashew-based cheeses.
Health Benefits of a Whole Food Plant-Based Diet
Heart Health: A plant-based diet has been shown to significantly reduce the risk of heart disease. It is low in saturated fats and cholesterol, which are often linked to cardiovascular issues. A diet rich in whole grains, fruits, vegetables, and legumes supports healthy cholesterol levels and blood pressure.
Weight Management: Whole food plant-based diets are naturally lower in calories and high in fibre, which can help in weight management. Fibre-rich foods promote a feeling of fullness, reducing overall calorie intake without the need for strict portion control.
Diabetes Prevention and Management: This diet has a low glycemic index, which helps regulate blood sugar levels. Studies have found that a plant-based diet can prevent and even reverse type 2 diabetes by improving insulin sensitivity and reducing blood sugar levels.
Reduced Risk of Cancer: Several studies have shown that diets rich in fruits, vegetables, and other plant foods are associated with a lower risk of certain types of cancer, including breast, prostate, and colorectal cancers.
Enhanced Digestion: The high fibre content in plant-based foods promotes healthy digestion by supporting a diverse gut microbiome. A healthy gut is linked to improved immunity and reduced inflammation.
Longevity: Populations that consume predominantly plant-based diets, such as those in the Blue Zones (regions with high life expectancy), tend to live longer and healthier lives. These diets provide essential nutrients, antioxidants, and anti-inflammatory compounds that contribute to overall well-being and longevity.
Did you know
In order to know what are the best foods, we must study God's original plan for man's diet. He who created man and who understands his needs appointed Adam his food. "Behold," He said, "I have given you every herb yielding seed, ... and every tree, in which is the fruit of a tree yielding seed; to you it shall be for food." Genesis 1:29, A.R.V. Upon leaving Eden to gain his livelihood by tilling the earth under the curse of sin, man received permission to eat also "the herb of the field." Genesis 3:18.
Grains, fruits, nuts, and vegetables constitute the diet chosen for us by our Creator. These foods, prepared in as simple and natural a manner as possible, are the most healthful and nourishing. They impart a strength, a power of endurance, and a vigor of intellect that are not afforded by a more complex and stimulating diet.
But not all foods wholesome in themselves are equally suited to our needs under all circumstances. Care should be taken in the selection of food. Our diet should be suited to the season, to the climate in which we live, and to the occupation we follow. Some foods that are adapted for use at one season or in one climate are not suited to another. So there are different foods best suited for persons in different occupations. Often food that can be used with benefit by those engaged in hard physical labor is unsuitable for persons of sedentary pursuits or intense mental application. God has given us an ample variety of healthful foods, and each person should choose from it the things that experience and sound judgment prove to be best suited to his own necessities. -EGW
Ensuring Nutrient Sufficiency on a Whole Food Plant-Based Diet
While a whole food plant-based diet offers a plethora of health benefits, it's important to ensure that all essential nutrients are consumed adequately. This can easily be achieved with mindful planning and a diverse diet that includes a wide range of plant foods. Here’s a closer look at some key nutrients to be aware of and how to incorporate them effectively into a plant-based diet:
Protein
Protein is a crucial macronutrient that supports muscle repair, immune function, and the production of enzymes and hormones. While plant-based sources of protein are abundant, it’s essential to consume a variety of them to ensure you're getting all the necessary amino acids, the building blocks of protein.
Sources of Plant-Based Protein: Legumes (such as beans, lentils, and chickpeas), tofu, tempeh, edamame, quinoa, nuts, seeds, and whole grains are excellent sources of plant-based protein. Including a variety of these foods throughout the day ensures you get a full spectrum of amino acids.
Vitamin B12
Vitamin B12 is crucial for nerve function, red blood cell formation, and DNA synthesis. It is primarily found in animal products, so those following a strictly plant-based diet need to be mindful of their B12 intake.
Sources of Vitamin B12: Plant-based eaters can obtain B12 through fortified foods like plant milks, cereals, and nutritional yeast or by taking a B12 supplement. It is important to regularly monitor B12 levels to avoid deficiencies or toxicity.
Iron
Iron is essential for transporting oxygen throughout the body and supporting immune function. Plant-based sources of iron (non-heme iron) are not absorbed as efficiently as the heme iron found in animal products, but there are ways to enhance absorption.
Sources of Iron: Lentils, chickpeas, beans, tofu, spinach, quinoa, pumpkin seeds, and fortified cereals are all rich in iron. Pairing these foods with vitamin C-rich foods, such as citrus fruits, strawberries, bell peppers, and tomatoes, can enhance iron absorption.
Calcium
Calcium is important for bone health, muscle function, and nerve signalling. While dairy products are a well-known source of calcium, there are plenty of plant-based sources as well.
Sources of Calcium: Leafy green vegetables (like kale, collard greens, and bok choy), fortified plant milks (such as almond, soy, and oat milk), tofu made with calcium sulfate, sesame seeds, chia seeds, and almonds are all excellent sources of calcium.
Omega-3 Fatty Acids
Omega-3 fatty acids are vital for brain health, reducing inflammation, and supporting heart health. While they are often associated with fish, plant-based eaters can obtain omega-3s from several sources.
Sources of Omega-3 Fatty Acids: Flaxseeds, chia seeds, walnuts, hemp seeds, and algae-based supplements are good sources of omega-3 fatty acids, particularly alpha-linolenic acid (ALA), which the body can convert into the active forms EPA and DHA, albeit at a lower efficiency.
Vitamin D
Vitamin D is important for bone health, immune function, and overall well-being. It is synthesized by the skin when exposed to sunlight, but factors such as geographic location, skin pigmentation, and sunscreen use can affect vitamin D synthesis.
Sources of Vitamin D: Limited plant-based food sources naturally contain vitamin D. However, fortified foods such as plant milks, cereals, and orange juice can help. A vitamin D supplement or adequate sun exposure is often recommended, especially during the winter months or in regions with limited sunlight.
Zinc
Zinc plays a crucial role in immune function, DNA synthesis, and cell division. While zinc is found in plant foods, its absorption can be inhibited by phytates, which are present in some grains and legumes.
Sources of Zinc: Whole grains, beans, lentils, chickpeas, seeds (especially pumpkin seeds), nuts, and tofu are all good sources of zinc. Soaking and sprouting grains and legumes can reduce phytate levels and enhance zinc absorption.
Iodine
Iodine is essential for thyroid function and metabolism. Since most plant foods are low in iodine, it’s important for those on a plant-based diet to ensure they are getting enough of this nutrient.
Sources of Iodine: Potatoes with the skin on, seaweed such as dulse and nori, tasty strawberries, dried prunes, and certain fortified foods are reliable sources of iodine. However, intake should be monitored because both deficiency and excess iodine can lead to thyroid issues.
Tips for a Nutrient-Dense Plant-Based Diet
To ensure nutrient sufficiency on a whole food plant-based diet, consider these additional tips:
Diverse Diet: Eat a variety of fruits, vegetables, grains, legumes, nuts, and seeds to cover a broad spectrum of nutrients.
Fortified Foods: Include fortified plant-based milks, cereals, and nutritional yeast in your diet to help meet nutritional needs for vitamins like B12 and D.
Whole Foods Over Processed: Prioritize whole, unprocessed foods over highly processed plant-based alternatives, which may lack nutrients and contain added sugars and unhealthy fats.
Mindful Supplementation: Consider supplements for nutrients that may be challenging to obtain solely from food, such as B12, vitamin D, and omega-3 fatty acids, particularly for those with specific dietary restrictions or limited sun exposure.
Regular Monitoring: Periodic blood tests can help track nutrient levels, allowing for adjustments in diet or supplementation as needed.
By focusing on nutrient-dense whole foods and mindful planning, a whole food plant-based diet can provide all the essential nutrients required for optimal health. This approach aligns with both ancient wisdom and modern science, demonstrating that a plant-based diet is not only sustainable but also highly beneficial for overall well-being.
Ancient Diets and Agricultural Practices
The idea of consuming a plant-based diet is not a modern trend. Long before the rise of contemporary dietary movements, ancient human societies primarily subsisted on plant-based foods. Archaeological findings from sites like Göbekli Tepe, a prehistoric site in modern-day Turkey dating back to around 9600 BC, provide a window into the dietary habits of early humans and highlight the central role of plants in their diets.
Göbekli Tepe and Early Human Diets
Göbekli Tepe is one of the most significant archaeological discoveries of the 20th century, shedding light on early human societies and their dietary practices. The site, which predates Stonehenge by about 6,000 years, offers evidence that early humans in this region consumed a predominantly plant-based diet.
Excavations at Göbekli Tepe have revealed an abundance of plant remains, including grains, nuts, fruits, and seeds, suggesting that these foods formed the backbone of the diet for those who inhabited or frequented the site. This evidence aligns with findings from other prehistoric sites, indicating that early human communities relied heavily on foraging and gathering to obtain food.
Grains: Archaeobotanical studies at Göbekli Tepe have uncovered large quantities of wild einkorn wheat, barley, and other grasses, indicating that these early humans gathered grains extensively. The presence of grinding stones and other processing tools at the site suggests that these grains were not only collected but also processed into flour or meal, which could be used in various forms, such as porridge or bread.
Fruits and Nuts: Remains of wild pistachios, almonds, and other nuts have been found at Göbekli Tepe, highlighting the importance of these nutrient-dense foods in the early human diet. Wild fruits such as grapes, figs, and berries were also likely consumed, providing essential vitamins and minerals.
Seeds: Seeds such as flax and wild legumes were also present at Göbekli Tepe, further supporting the idea that early humans had a diet rich in plant-based foods. These seeds would have provided essential fatty acids, proteins, and other nutrients necessary for survival.
The Role of Foraging and Early Agriculture
Before the full advent of agriculture, early humans were primarily foragers, relying on their knowledge of the local environment to find edible plants, fruits, nuts, and seeds. This lifestyle required a deep understanding of seasonal cycles, plant growth patterns, and ecological relationships, which enabled them to harvest a diverse array of plant foods throughout the year.
As these early human societies began to experiment with cultivation, they laid the foundations for agriculture. The transition to farming was gradual and occurred independently in different regions around the world, including the Fertile Crescent, where Göbekli Tepe is located. The domestication of wild plants such as einkorn wheat and barley marked the beginning of a shift toward more settled, agrarian lifestyles.
Cultivation of Grains and Legumes: The early cultivation of grains and legumes was a game-changer for human societies. These crops provided a reliable and storable food source that could sustain populations through seasonal shortages or unpredictable weather conditions. Grains like wheat and barley, along with legumes such as lentils and chickpeas, became staple foods that could be cultivated in a variety of environments, contributing to the growth and stability of early agricultural communities.
Development of Farming Techniques: With the advent of farming, humans began to develop techniques for planting, cultivating, and harvesting crops. This included the selective breeding of plants to enhance desirable traits such as yield, size, and taste. As a result, the variety and abundance of plant-based foods increased, further solidifying their central role in the human diet.
Agriculture and the Adaptation of Human Diets
The development of agriculture had profound implications for human adaptation and the structure of societies. As plant-based foods became more abundant and reliable through farming, early human societies could support larger populations and more complex social structures. This period saw the establishment of permanent settlements, the rise of cities, and the development of trade networks, all of which were underpinned by the agricultural production of plant-based foods.
Impact on Health and Nutrition: The shift to agriculture brought about significant changes in human health and nutrition. While agriculture allowed for a more stable food supply, it also led to a diet that was more reliant on a narrower range of foods. The reduction in dietary diversity and the increase in carbohydrate-heavy crops, such as grains, may have contributed to declines in nutritional status and increases in certain health conditions, such as dental caries (tooth decay) and nutritional deficiencies.
Cultural and Societal Impacts: The centrality of plant-based foods in ancient agricultural societies also shaped cultural and societal norms. Many ancient civilizations revered certain crops, such as wheat in ancient Egypt or rice in East Asia, as sacred or essential to their way of life. The cultivation, harvesting, and consumption of these crops were often embedded in religious practices, social rituals, and economic systems.
Legacy of Ancient Plant-Based Diets
The plant-based diets of our ancient ancestors have left a lasting legacy on human societies. The cultivation of grains, fruits, vegetables, nuts, and seeds formed the backbone of early agriculture and continues to be a fundamental component of modern diets. Today, there is a growing recognition of the health benefits associated with plant-based eating, echoing the dietary practices of ancient human societies.
Modern research supports the idea that a diet rich in whole, unprocessed plant foods can promote health and prevent chronic diseases. By looking to the past and understanding the dietary patterns of our ancestors, we can gain valuable insights into the benefits of plant-based diets and the importance of returning to a more natural and balanced way of eating.
By exploring the ancient diets and agricultural practices of our ancestors, we can better understand the origins of our food systems and the enduring significance of plant-based diets.
Conclusion
In conclusion, a whole food plant-based diet is about embracing the nourishing power of foods in their most natural state, focusing on the plant-based ingredients that fuel our bodies with essential nutrients for vibrant health. This way of eating is a return to simplicity, rooted in the wisdom of ancient traditions that have sustained humanity for generations. By making this choice, you're not only investing in your well-being but also honouring the legacy of our ancestors and, most importantly, the design God has for us.
We have a duty to honour God by caring for the bodies He entrusted to us, nurturing ourselves with the best that nature has to offer, and setting an example of health and stewardship for others. Let this journey towards a whole food plant-based diet be a testament to your commitment to health, faith, and community.
Take the first step today—nourish your body, care for the planet, and reflect God's love in your actions. After all, our diet is not just a personal choice; it’s an expression of respect for God, ourselves, and those around us.
Continue to scrolling for a special treat at the end.
References
2. Journal of General Internal Medicine
3. National Institutes of Health (NIH) - Vitamin B12
4. National Institutes of Health (NIH) - Calcium
5. National Institutes of Health (NIH) - Vitamin D
7. Satija, A., Bhupathiraju, S. N., Spiegelman, D., Chiuve, S. E., Manson, J. E., Willett, W., ... & Hu, F. B. (2017). "Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults." _Journal of the American College of Cardiology, 70_(4), 411-422. Available from: [JACC Journal]
8. Dietrich, O., Heun, M., Notroff, J., Schmidt, K., & Zarnkow, M. (2012). "The Role of Cultivation in Early Neolithic Ritual Practices: The Case of Göbekli Tepe." _Current Anthropology, 53_(6), 396-433. Available from: [University of Chicago Press]
9. Price, T. D., & Bar-Yosef, O. (Eds.). (2011). The Origins of Agriculture: New Data, New Ideas. University College London. Available from: [University College London Press]
10. T. Colin Campbell Center for Nutrition Studies. "What is a Whole Food, Plant-Based Diet?" Available from: [Nutrition Studies]
11. Dietrich, O., Heun, M., Notroff, J., Schmidt, K., & Zarnkow, M. (2012). "The Role of Cultivation in Early Neolithic Ritual Practices: The Case of Göbekli Tepe." _Current Anthropology, 53_(6), 396-433. Available from: [University of Chicago Press]
12. Katz, S. H., & Voigt, M. M. (1986). "Bread and Beer: The Early Use of Cereals in the Human Diet." _Expedition, 28_(2), 23-34. Available from: [University of Pennsylvania Museum of Archaeology and Anthropology]
13. Processed and Refined Foods
Research shows that highly processed foods are linked to inflammation, weight gain, and chronic diseases.
Harvard T.H. Chan School of Public Health. (n.d.). "Processed Foods and Health."
Available at: Harvard School of Public Health
14. Refined Grains
Refined grains can lead to spikes in blood sugar and increase the risk of chronic disease.
The Nutrition Source, Harvard T.H. Chan School of Public Health. (n.d.). "Whole Grains."
Available at: Harvard School of Public Health
15. Added Sugars and Sweeteners
High sugar intake is associated with weight gain, type 2 diabetes, and heart disease.
World Health Organization (WHO). (2015). "Guideline: Sugars Intake for Adults and Children."
Available at: World Health Organization
16. Oils and Fats
Research links high intake of refined oils to weight gain and heart disease.
National Institutes of Health (NIH). (n.d.). "Dietary Fats."
Available at: NIH Office of Dietary Supplements
17. Animal Products
Reducing or eliminating animal products can lower the risk of chronic diseases.
American Heart Association (AHA). (2019). "The Benefits of Plant-Based Diets."
Available at: American Heart Association
18. Processed Plant-Based Meats and Dairy Alternatives
While convenient, processed plant-based alternatives are often high in sodium and additives.
Harvard T.H. Chan School of Public Health. (n.d.). "The Truth About Plant-Based Meat."
Available at: Harvard School of Public Health
Stay healthy and vibrant!
No Bake Cheesecake
Crust
Ingredients
▢2/3 cup pecans
▢1/3 cup walnuts
▢8-10 Medjool dates (I used 1 cup about 20 deglet noor dates)
▢1/4 cup unsweetened coconut flakes ( I omitted this ingredient)
▢1/4 teaspoon kosher salt (I used pink Himalayan salt)
Instructions
Crust
1. Combine the nuts in a food processor and pulse until you get a coarse mixture. Add the rest of the crust ingredients and pulse several times until it starts clumping up and forming together. (Soak dates in your water for like 10 or so minutes so it's soft. Then drain and add to the processor with the nuts and pulse until combined)
2. Place the crust mix in a pie dish and using your hands and or spatula spread the mix evenly to form a crust alongside the entire pie dish.
For the filling
Ingredients
▢ 32 ounces (4 8-ounce packages) vegan cream cheese (if you need to add another 8 ounces of cream cheese)
▢ (1) 13.5 ounce can coconut cream (full fat not boxed as it can contain too much water)
▢ 1 1/4 cups granulated sugar (I used 1 cup Rapadura sugar and 1/4 cup agave)
▢ 1 1/2 teaspoon agar powder (not flakes and this ingredient CANNOT be substitutd because it acts as a thickening agent)
▢ 2 teaspoons pure vanilla extract
▢ 3 tablespoons lemon juice, from about 2 small lemons
Instructions
For the filling
1. In the bowl of an electric mixer with the whisk attachment, or using a handheld mixer, beat the vegan cream cheese and coconut cream until smooth, about 1 minute.
2. Now add the rest of the filling ingredients and beat until smooth, scraping down the sides and bottom of the bowl as needed.
3. Pour the filling over the crust. Tap on the counter a couple of times to release any air bubbles that may have formed. Cover lightly with plastic wrap and seal the top with aluminum foil. Let it set in the freezer for 4-6 hours or untill the filling is at desired texture.
4. When ready to serve, pull out the cheesecake and allow it to sit at room temperature for about 10-15 minutes before slicing and serving. Top off with sauce.
Fruit Glaze Sauce
Ingredients
▢ 1 pound strawberries sliced ( I used 70% frozen strawberries and 30% mixed berry frozen fruit)
▢ 1/4 cup water
▢ 1 ½ teaspoons lemon juice
▢ 1/4 cup sugar (Rapadura)
For thickening the sauce
▢ 1 tablespoon corn starch (arrowroot)
▢ 1 tablespoon water
Instructions
Fruit glaze sauce
1. In a large saucepan over high heat, add strawberries, water, sugar, and lemon juice. Stir to mix and bring it to a boil.
2. Reduce the heat and simmer for 10 minutes or until the strawberries become soft.
3. Remove from heat and blend the strawberries gently (I used immersion blender.)
4. Strain the mixture through a strainer. (I omitted this process)
5. Then pour the liquid back to the saucepan on low heat.
Instructions continued
1. In a small bowl, mix together corn starch with 1 tablespoon of water.
2. Pour the corn starch slurry into the simmering strawberry sauce. Stir constantly.
3. Increase the heat to high, keep whisking for about 5 minutes or until it thickens into a glaze.
4. Remove from heat, and pour it into a bowl or container to cool down.
5. Once it comes down to room temperature, store it in the refrigerator. Serve it as a topping for cheesecake, donuts, and pie, etc.
Embrace this colourful, healthful journey and experience the transformative power of a whole food plant-based diet!
DISCLAIMER: The health information in this blog is for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Unlocking Health with GI-MAP Testing: A Deep Dive into Your Gut Health
Unlocking Health with GI-MAP Testing: A Deep Dive into Your Gut Health
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, my mission is to help you uncover the root causes of your health challenges so you can achieve true wellness. One of the most powerful tools I use in my practice is the GI-MAP (Gastrointestinal Microbial Assay Plus) test—a cutting-edge stool analysis that provides deep insights into your gut health.
Your gut is the foundation of your overall health, influencing everything from digestion to immune function, mental well-being, and even hormone balance. When the delicate balance of your gut microbiome is disrupted—a condition known as gut dysbiosis—it can lead to a host of issues, including bloating, fatigue, skin problems, and chronic inflammation. But the impact doesn’t stop there. The gut is intricately connected to your hormone health, playing a crucial role in regulating everything from estrogen and cortisol to insulin and thyroid hormones.
In this blog, I’ll share why I use GI-MAP testing in my practice and how it helps identify the root causes of gut issues and hormonal imbalances, paving the way for personalized, effective healing strategies. Whether you’re dealing with digestive discomfort, hormonal imbalances, or just feeling "off," understanding your gut health could be the key to unlocking optimal wellness.
Why Gut Health Matters
The gut is often referred to as the "second brain" because it plays a crucial role in overall health and well-being. It is home to trillions of bacteria, viruses, and fungi—collectively known as the gut microbiome. This complex ecosystem influences not only digestion but also immune function, mood, energy levels, and even skin health. When the balance of the microbiome is disrupted, it can lead to a host of health issues, including digestive disorders, autoimmune diseases, chronic fatigue, and more.
The Science Behind GI-MAP Testing
The GI-MAP (Gastrointestinal Microbial Assay Plus) is a cutting-edge stool test that uses quantitative PCR (qPCR) technology to analyze the DNA of microorganisms present in your gut. This advanced method allows for the precise identification and quantification of various pathogens, beneficial bacteria, parasites, viruses, and fungi that may be impacting your health.
Pathogen Identification: GI-MAP testing is highly effective in detecting bacterial, viral, and parasitic pathogens that can cause or contribute to gastrointestinal symptoms. For example, a study published in Clinical Infectious Diseases highlights how qPCR technology used in GI-MAP can accurately detect Clostridium difficile infections, which are often missed by conventional methods.
Microbiome Imbalances: The test provides detailed information about the balance of beneficial and harmful bacteria in your gut. A healthy gut typically has a high diversity of beneficial bacteria, such as Lactobacillus and Bifidobacterium. When these populations are depleted or outnumbered by harmful bacteria, it can lead to dysbiosis, which has been linked to conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and even mental health disorders like depression and anxiety.
Inflammation Markers: GI-MAP also measures markers of inflammation, such as calprotectin, which can indicate the presence of inflammatory bowel diseases like Crohn’s disease and ulcerative colitis. Elevated levels of calprotectin have been shown to correlate with increased gut inflammation, providing a clear indicator of underlying issues.
Immune Function: Secretory IgA (sIgA) is another crucial marker included in the GI-MAP test. sIgA is the first line of defense in the gut, protecting against pathogens and maintaining a healthy gut lining. Low levels of sIgA may indicate chronic stress or a weakened immune response, leaving the gut vulnerable to infections and inflammation.
Digestive Function: The test also assesses digestive markers such as pancreatic elastase, which is essential for proper digestion. Low levels of pancreatic elastase can indicate exocrine pancreatic insufficiency, a condition where the pancreas does not produce enough enzymes to digest food properly, leading to malabsorption and nutrient deficiencies.
The Impact of GI-MAP Results on Health Outcomes
The detailed insights provided by the GI-MAP test allow for personalized treatment plans tailored to each individual's unique needs. For instance, if the test reveals an overgrowth of pathogenic bacteria like H. pylori, which has been linked to ulcers and stomach cancer, a targeted protocol involving specific herbal antimicrobials, probiotics, and dietary changes can be implemented to restore balance and alleviate symptoms.
Similarly, if a client presents with chronic diarrhea and the GI-MAP test detects the presence of Giardia, a common parasitic infection, we can design a treatment plan that includes anti-parasitic herbs and supplements to eradicate the infection and support the healing of the gut lining.
In addition, by identifying and addressing imbalances in beneficial bacteria, we can help clients manage or even resolve chronic conditions such as IBS. A study published in the World Journal of Gastroenterology found that patients with IBS who received targeted probiotic therapy based on stool test results experienced significant improvements in symptoms compared to those who received a placebo.
The Gut-Hormone Connection: How GI-MAP Testing Can Help Address Hormonal Imbalances
When people think about hormones, they often focus on glands like the thyroid, ovaries, or adrenal glands. However, the gut plays a crucial role in regulating hormones, making gut health essential for hormonal balance. The GI-MAP (Gastrointestinal Microbial Assay Plus) test, a comprehensive stool analysis, provides insights that can be instrumental in identifying and addressing hormonal imbalances.
Fun Fact
Fun Fact: The GI-MAP test by Diagnostic Solutions Laboratory is one of the few gut health assessments that uses advanced quantitative PCR (qPCR) technology, allowing it to precisely measure the DNA of bacteria, viruses, fungi, and parasites in your gut. This technology provides highly accurate results, even at low levels of microbial presence, making it a powerful tool for detecting subtle imbalances that other tests might miss.
The Gut Microbiome's Role in Hormonal Balance
The gut microbiome influences hormone levels through several mechanisms:
1. Estrogen Metabolism: One of the most well-researched connections between gut health and hormones is the gut's role in estrogen metabolism. The estrobolome, a subset of gut bacteria, is responsible for metabolizing estrogen. If the estrobolome is imbalanced—due to an overgrowth of harmful bacteria or a lack of beneficial ones—estrogen metabolism can be disrupted. This can lead to either estrogen dominance, which is linked to conditions like PMS, fibroids, and breast cancer, or estrogen deficiency, which can contribute to osteoporosis and other issues.
2. Cortisol and Stress Response: The gut microbiome also influences the hypothalamic-pituitary-adrenal (HPA) axis, which controls the body's stress response and cortisol production. Dysbiosis, or an imbalance in the gut microbiome, can contribute to chronic stress and elevated cortisol levels, which in turn can lead to adrenal fatigue and other hormonal imbalances, such as thyroid dysfunction.
3. Insulin Sensitivity: Gut health impacts insulin sensitivity, which is crucial for regulating blood sugar levels and preventing insulin resistance—a key factor in conditions like polycystic ovary syndrome (PCOS) and type 2 diabetes. Studies have shown that certain gut bacteria play a role in glucose metabolism and can influence insulin signaling pathways.
4. Thyroid Function: Gut health can also affect thyroid function. For example, gut dysbiosis can lead to increased intestinal permeability (leaky gut), which allows endotoxins to enter the bloodstream. These endotoxins can trigger inflammation and immune responses that may contribute to thyroid conditions like Hashimoto's thyroiditis, an autoimmune thyroid disorder.
How GI-MAP Testing Can Help
GI-MAP testing provides detailed information about the gut microbiome and other digestive markers, offering insights that can help address hormonal imbalances:
1. Estrogen Metabolism Analysis: By evaluating the balance of gut bacteria, the GI-MAP test can provide clues about the estrobolome's health. If the test reveals an overgrowth of certain bacteria like Clostridia species, which are known to affect estrogen metabolism, targeted interventions such as probiotics, prebiotics, or antimicrobial herbs can be used to restore balance and improve estrogen metabolism.
2. Cortisol and Stress Markers: GI-MAP includes markers such as Secretory IgA (sIgA), which reflects the state of the gut's immune function and its response to stress. Low levels of sIgA can indicate chronic stress, which may be contributing to elevated cortisol levels. By addressing gut health, we can help modulate the stress response and support adrenal health.
3. Insulin Sensitivity Support: The test can identify imbalances in gut bacteria that are known to influence insulin sensitivity. For example, an overgrowth of Firmicutes relative to Bacteroidetes has been linked to obesity and insulin resistance. Correcting these imbalances through dietary changes and specific probiotics can help improve insulin sensitivity, which is crucial for managing conditions like PCOS.
4. Thyroid Function and Gut Health: GI-MAP can detect gut pathogens, dysbiosis, and markers of inflammation that may be contributing to thyroid dysfunction. By addressing these gut issues, we can reduce the inflammatory burden on the body and support healthier thyroid function.
Case Study: GI-MAP and Hormonal Balance
Consider a client who has been struggling with symptoms of estrogen dominance, such as heavy periods, breast tenderness, and mood swings. Despite trying various hormonal treatments, her symptoms persist. After conducting a GI-MAP test, we discover she has dysbiosis with an overgrowth of Beta-glucuronidase-producing bacteria. Beta-glucuronidase is an enzyme that reactivates estrogen in the gut, leading to higher circulating levels of estrogen.
With this information, we implement a protocol to reduce the overgrowth, including specific probiotics, dietary changes, and the use of calcium D-glucarate, a supplement known to inhibit Beta-glucuronidase. Over the next few months, the client experiences significant relief from her symptoms as her estrogen levels normalize.
A Client Success Story
To illustrate the power of GI-MAP testing, let me share a success story from my practice. A client came to me after years of struggling with bloating, fatigue, and brain fog. She had seen multiple doctors, tried various diets, and taken countless supplements with little to no improvement. After conducting a GI-MAP test, we discovered that she had an overgrowth of Klebsiella pneumoniae, a pathogenic bacterium associated with inflammation and gut permeability, along with low levels of beneficial bacteria and elevated calprotectin.
Based on these results, we implemented a comprehensive plan that included antimicrobial herbs to target the Klebsiella, high-quality probiotics to replenish beneficial bacteria, and anti-inflammatory supplements to reduce gut inflammation. Within a few months, her symptoms improved dramatically—her bloating was gone, her energy levels increased, and she experienced greater mental clarity.
Conclusion: Take Control of Your Health with GI-MAP Testing
If you’ve been struggling with chronic health issues and haven’t found answers, GI-MAP testing could be the missing piece of the puzzle. By uncovering the root causes of your symptoms, this advanced stool test empowers you to take control of your health and start the journey toward healing.
As a practitioner dedicated to helping you achieve optimal health, I’m here to guide you every step of the way. If you’re ready to get to the root of your health challenges and reclaim your vitality, contact me today to schedule a consultation and learn more about how GI-MAP testing can benefit you.
Together, we can unlock the secrets of your gut health and pave the way for a healthier, happier you.
References:
1. Persson, S., Torpdahl, M., Olsen, K. E., & Christensen, J. J. (2008). "Detection of Clostridium difficile in Feces by Real-Time PCR." Clinical Infectious Diseases, 46(Supplement_1), S32-S36. https://doi.org/10.1086/521863
2. Carding, S., Verbeke, K., Vipond, D. T., Corfe, B. M., & Owen, L. J. (2015). "Dysbiosis of the gut microbiota in disease." Microbial Ecology in Health and Disease, 26(1), 26191. https://doi.org/10.3402/mehd.v26.26191
3. Dinan, T. G., & Cryan, J. F. (2017). "The microbiome-gut-brain axis in health and disease." Gastroenterology Clinics of North America, 46(1), 77-89. https://doi.org/10.1016/j.gtc.2016.09.007
4. Walsham, N. E., & Sherwood, R. A. (2016). "Fecal calprotectin in inflammatory bowel disease." Clinical and Experimental Gastroenterology, 9, 21-29. https://doi.org/10.2147/CEG.S51902
5. Brandtzaeg, P. (2013). "Secretory IgA: Designed for anti-microbial defense.” Frontiers in Immunology, 4, 222. https://doi.org/10.3389/fimmu.2013.00222
6. Loser, C. (2010). "Exocrine pancreatic insufficiency – a neglected diagnosis." Dtsch Arztebl Int, 107(34-35), 577-582. https://doi.org/10.3238/arztebl.2010.0577
7. Buzás, G. M. (2010). "Helicobacter pylori—an overview." Scandinavian Journal of Gastroenterology, 45(1), 3-9. https://doi.org/10.3109/00365520903431737
8. Thompson, R. C., & Monis, P. T. (2012). "Giardiasis: An update on transmission, diagnosis, and drug resistance." Infectious Disease Clinics of North America, 26(2), 253-268. https://doi.org/10.1016/j.idc.2012.03.001
9. Ford, A. C., Harris, L. A., Lacy, B. E., & Quigley, E. M. (2020). "Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome." Alimentary Pharmacology & Therapeutics, 52(7), 637-652. https://doi.org/10.1111/apt.15932
GI-Map and Hormones reference:
1. Plottel, C. S., & Blaser, M. J. (2011). "Microbiome and malignancy." Cell Host & Microbe, 10(4), 324-335. https://doi.org/10.1016/j.chom.2011.10.003
2. De Palma, G., Collins, S. M., Bercik, P., & Verdu, E. F. (2014). "The microbiota-gut-brain axis in gastrointestinal disorders: stressed bugs, stressed brain or both?" Journal of Physiology, 592(14), 2989-2997. https://doi.org/10.1113/jphysiol.2014.273789
3. Shreiner, A. B., Kao, J. Y., & Young, V. B. (2015)."The gut microbiome in health and in disease." Current Opinion in Gastroenterology, 31(1), 69-75. https://doi.org/10.1097/MOG.0000000000000139
4. Cryan, J. F., & Dinan, T. G. (2012). "Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour." Nature Reviews Neuroscience, 13(10), 701-712. https://doi.org/10.1038/nrn3346
5. Vrieze, A., Out, C., Fuentes, S., Jonker, L., Reuling, I. E., Kootte, R. S., ... & Hoekstra, J. B. (2014). "Impact of oral vancomycin on gut microbiota, bile acid metabolism, and insulin sensitivity." Journal of Hepatology, 60(4), 824-831. https://doi.org/10.1016/j.jhep.2013.11.034
6. Fasano, A. (2012). “Leaky gut and autoimmune diseases." Clinical Reviews in Allergy & Immunology, 42(1), 71-78. https://doi.org/10.1007/s12016-011-8291-x
Bacterial species and their relevance to gut health:
1. Lactobacillus and Bifidobacterium:
Lactobacillus and Bifidobacterium are beneficial bacteria that play a crucial role in maintaining a healthy gut microbiome. They help with digestion, boost immune function, and protect against harmful pathogens.
“The Role of Lactobacillus and Bifidobacterium in the Gut Microbiome.” International Scientific Association for Probiotics and Prebiotics (ISAPP). [https://isappscience.org/the-role-of-lactobacillus-and-bifidobacterium-in-the-gut-microbiome/].
2. Clostridia Species:
Clostridia species are a group of bacteria that can include both beneficial and harmful types. Some species are involved in the fermentation of dietary fibers, producing beneficial short-chain fatty acids, while others can be pathogenic and produce toxins.
“Clostridia: A Mixed Bag of Gut Microbes.” Gut Microbiota Worldwatch. [http://www.gutmicrobiotawatch.org/clostridia-mixed-bag-gut-microbes/].
3. Firmicutes Relative to Bacteroidetes:
The balance between Firmicutes and Bacteroidetes is crucial for maintaining a healthy gut microbiome. An overgrowth of Firmicutes relative to Bacteroidetes has been linked to obesity and metabolic disorders.
“The Firmicutes/Bacteroidetes Ratio: A Key Player in Obesity and Gut Health.” American Society for Microbiology (ASM). [https://www.asm.org/Articles/2020/June/The-Firmicutes-Bacteroidetes-Ratio-Key-Player-in].
4. Beta-glucuronidase:
Beta-glucuronidase is an enzyme produced by certain gut bacteria that can reactivate hormones like estrogen, affecting their balance in the body. High levels of this enzyme are often associated with conditions like estrogen dominance.
“Beta-Glucuronidase: A Double-Edged Sword in Gut Health.” Clinical Education. [https://www.clinicaleducation.org/resources/reviews/beta-glucuronidase-a-double-edged-sword-in-gut-health/].
5. Klebsiella pneumoniae:
Klebsiella pneumoniae is a type of bacteria that can be part of the normal gut flora but may become pathogenic under certain conditions, contributing to gut dysbiosis, inflammation, and conditions like rheumatoid arthritis.
“Klebsiella pneumoniae: From Commensal Gut Bacteria to Pathogen.” Centers for Disease Control and Prevention (CDC). [https://www.cdc.gov/klebsiella/index.html].
This explanation and the references provided demonstrate the interconnectedness of gut health and hormonal balance, emphasizing how GI-MAP testing can be a valuable tool in identifying and addressing these issues.
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Nurturing Gut Health for Total Wellness: A Comprehensive Guide
Nurturing Gut Health for Total Wellness: A Comprehensive Guide
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, I am thrilled to guide you through the fascinating world of gut health—a cornerstone of our overall well-being. Did you know that the state of your gut can influence everything from your immune function and hormone balance to your mental clarity and emotional resilience? It’s true! Our gut is often called our "second brain," and for a good reason. It plays a crucial role in almost every aspect of our health.
In this comprehensive guide, we'll explore how nurturing your gut can transform your life. Whether you’re dealing with digestive discomfort, seeking better energy levels, or looking to boost your mood and immune system, focusing on gut health is a great place to start. We'll dive deep into understanding the difference between good and bad bacteria, what causes imbalances, and, most importantly, how to restore harmony in your digestive system.
Grab a cup of herbal tea, settle in, and let’s embark on this journey to nurturing your gut and achieving total wellness together!
The Difference Between Good and Bad Bacteria
Your gut is home to a vast community of microorganisms, including bacteria, viruses, fungi, and other microbes, collectively known as the gut microbiome. Among these, bacteria play a significant role in your health.
Good Bacteria: Beneficial bacteria, often referred to as probiotics, are crucial for maintaining gut health. They aid in digestion, produce essential vitamins (like vitamin K and certain B vitamins), support the immune system, and protect the gut lining from harmful invaders. Common beneficial strains include Lactobacillus and Bifidobacterium, which are found in fermented foods such as yogurt, kefir, sauerkraut, and kimchi, as well as in high-quality probiotic supplements.
Bad Bacteria: On the flip side, harmful bacteria can cause a range of issues when they grow out of balance. These pathogens can produce toxins, trigger inflammation, and damage the gut lining, leading to conditions like leaky gut syndrome. Some common harmful bacteria include specific strains of Escherichia coli (E. coli), Clostridium difficile (C. diff), and Salmonella.
What Causes an Imbalance of Bad Bacteria?
An imbalance in your gut microbiome, known as dysbiosis, can be triggered by various factors. Here are some common causes:
1. Poor Diet: Diets high in refined sugars, processed foods, and unhealthy fats can feed harmful bacteria and yeast, leading to an overgrowth. For instance, studies have shown that a diet rich in sugar and fat can alter the composition of gut bacteria, promoting the growth of harmful species like Firmicutes while decreasing beneficial Bacteroidetes.
2. Antibiotic Overuse: While antibiotics are sometimes necessary, they can disrupt the gut microbiome by killing off both good and bad bacteria. This leaves room for opportunistic pathogens to take over. Research has shown that even short courses of antibiotics can significantly reduce microbial diversity in the gut, with effects that may last for months or even years.
3. Chronic Stress: Stress has a profound impact on the gut. It can alter gut motility, increase gut permeability (leading to leaky gut), and change the composition of the gut microbiota. Chronic stress has been linked to a decrease in beneficial bacteria like Lactobacillus and an increase in harmful bacteria.
4. Lack of Sleep: Poor sleep disrupts the natural circadian rhythms that govern your gut. Studies have shown that irregular sleep patterns can lead to an imbalance in the gut microbiome, potentially contributing to metabolic disorders like obesity and diabetes.
5. Environmental Toxins: Exposure to environmental toxins, such as pesticides, heavy metals, and chemicals found in food and water, can negatively impact gut health. These toxins can disrupt the microbial balance, damage the gut lining, and trigger systemic inflammation.
Fun Fact
Did you know that the human gut microbiome is so unique that it's often referred to as your "second fingerprint"? No two people have the exact same composition of gut bacteria, even identical twins! This microbial "fingerprint" plays a crucial role in your digestion, immune system, and even mood, highlighting just how personalized our internal ecosystems truly are.
How to Improve Good Bacteria
Restoring a healthy balance of good bacteria in your gut requires a multifaceted approach. Here’s how you can nurture your gut microbiome:
1. Adopt a Whole Food, Plant-Based Diet: A diet rich in diverse, fiber-packed plants is one of the best ways to support a healthy gut. Fiber acts as a prebiotic, feeding the good bacteria in your gut. Foods like leafy greens, fruits, vegetables, legumes, and whole grains are excellent sources. A study published in the journal Nutrients found that a diet high in plant-based foods increases microbial diversity and promotes the growth of beneficial bacteria.
2. Incorporate Fermented Foods: Fermented foods are naturally rich in probiotics, which can help replenish and diversify your gut bacteria. Sauerkraut, kimchi, kefir, kombucha, and miso are great choices. Research has shown that regular consumption of fermented foods can increase the abundance of beneficial bacteria like Lactobacillus and Bifidobacterium.
3. Limit Processed Foods and Sugar: Processed foods and sugars promote the growth of harmful bacteria and yeast, which can lead to dysbiosis. By reducing these foods in your diet, you can help prevent the overgrowth of bad bacteria. A study in the British Journal of Nutrition found that diets high in refined carbohydrates and sugars are linked to increased gut inflammation and reduced microbial diversity.
4. Take a High-Quality Probiotic Supplement: Not all probiotics are created equal. Look for a supplement with multiple strains, including Lactobacillus and Bifidobacterium, and ensure it comes from a reputable source. Probiotic supplements can help restore balance, especially after a course of antibiotics or during periods of high stress.
5. Use Herbs and Spices: Certain herbs and spices have antimicrobial properties that can help keep harmful bacteria in check while supporting overall gut health. Garlic, ginger, turmeric, and oregano are particularly effective. For example, turmeric has been shown to enhance the growth of beneficial bacteria while inhibiting the growth of pathogens.
6. Stay Hydrated: Water is essential for maintaining the mucosal lining of the intestines, which acts as a barrier against harmful bacteria. Proper hydration also supports digestion and helps prevent constipation, which can contribute to dysbiosis .
The Role of Gut Health in Hormone Balance, Disease Prevention, and Emotional Well-being
Your gut is often referred to as your “second brain” because of its profound connection to other systems in the body, including the endocrine (hormonal) and nervous systems. Here’s how gut health influences various aspects of your health:
1. Hormone Balance: Your gut bacteria play a role in the production and regulation of hormones. For example, certain gut bacteria help metabolize and regulate estrogen levels. Dysbiosis can lead to hormonal imbalances, contributing to conditions like PMS, PCOS, and even infertility.
2. Disease Prevention: A healthy gut helps protect against chronic diseases, including autoimmune conditions, obesity, diabetes, and cardiovascular disease. The gut barrier prevents toxins and pathogens from entering the bloodstream and triggering inflammation, which is a root cause of many chronic diseases.
3. Emotional and Mental Well-being: The gut-brain axis is a bidirectional communication network between the gut and the brain. An imbalance in gut bacteria can influence mood, stress levels, and mental health conditions like anxiety and depression. Studies have shown that probiotics can help alleviate symptoms of depression and anxiety by modulating the gut microbiome.
How a Healthy Gut Enhances Quality of Life
When your gut is healthy, every part of your life improves. You’ll experience better digestion, enhanced nutrient absorption, more energy, clearer skin, and improved mental clarity. A balanced gut microbiome also supports a strong immune system, helping you fend off infections and recover more quickly from illness. Simply put, a healthy gut is foundational to feeling your best every day.
Functional Labs to Get to the Root Cause
Understanding your unique gut health requires more than just guessing—it requires data. Functional labs can provide insights into your gut microbiome and identify underlying issues. Here are some key tests:
1. Comprehensive Stool Analysis: This test evaluates your gut bacteria, including the balance of good and bad strains, the presence of parasites, yeast overgrowth, and digestive function markers like pancreatic elastase.
2. Organic Acids Test (OAT): This urine test detects metabolic byproducts that can indicate bacterial or fungal overgrowth, nutrient deficiencies, and oxidative stress in the body.
3. Food Sensitivity Testing: Identifying foods that trigger an immune response can help reduce inflammation and support gut healing.
4. Mucosal Barrier Assessment: Also known as an intestinal permeability test, this test measures the ability of your gut lining to function as a barrier, which is crucial for preventing toxins from entering the bloodstream.
A Comprehensive Gut Health Protocol
Step 1: Labs
Start with a comprehensive stool analysis, OAT, food sensitivity, and mucosal barrier assessment to identify imbalances and underlying issues.
Step 2: Supplements and Nutrients
- Probiotics: Choose a multi-strain probiotic from a reputable brand.
- L-Glutamine: Supports gut lining repair.
- Digestive Enzymes: Aid in breaking down food and improving nutrient absorption.
- Omega-3 Fatty Acids: Reduce inflammation and support gut health.
- Herbs: Consider supplements like turmeric, garlic, and ginger to support microbial balance.
Where to buy:
International code KXCTGG
Step 3: Diet
Follow a whole food, plant-based diet rich in fiber, fermented foods, and anti-inflammatory herbs and spices. Limit processed foods, sugars, and alcohol.
Step 4: Rest and Stress Reduction
Prioritize sleep and stress management techniques such as mindfulness, meditation, or stretching to support your gut-brain axis.
Step 5: Positive Attitude and Mindfulness
Cultivate a positive mindset and practice mindfulness to further support your gut health. The gut-brain connection means that your mental state can directly impact your gut microbiome. Regular mindfulness practices, such as meditation, deep breathing exercises, or spending time in nature, can help reduce stress and promote a balanced gut.
How to Implement This Protocol
1. Start with Testing: Schedule functional lab tests to get a clear picture of your gut health. This will help tailor your protocol to your specific needs.
2. Incorporate Supplements: Based on your lab results and personal health needs, introduce the recommended supplements to support gut healing and microbial balance.
3. Revamp Your Diet: Transition to a whole food, plant-based diet. Start by gradually replacing processed foods with nutrient-dense options like vegetables, fruits, legumes, nuts, seeds, and whole grains. Incorporate fermented foods daily to naturally boost your probiotic intake.
4. Focus on Lifestyle: Make sleep a priority by establishing a regular sleep schedule and creating a relaxing bedtime routine. Incorporate stress-reducing activities into your daily routine, such as stretching, meditation, or even a simple daily walk.
5. Practice Mindfulness: Set aside time each day for mindfulness practices that resonate with you. This could be as simple as mindful eating, where you focus on enjoying each bite of your food, or practicing gratitude before bed.
Call to Action
Your journey to optimal health begins in the gut. By taking these steps to balance your gut microbiome, you’re not just improving your digestion—you’re enhancing your overall quality of life. I encourage you to start with functional lab testing to uncover the root causes of any imbalances and to work with a knowledgeable practitioner who can guide you through this personalized journey.
If you’re ready to take charge of your health and transform your well-being from the inside out, I invite you to schedule a Complementary Discovery Call. Together, we’ll create a customized gut health plan tailored to your unique needs, with functional lab testing, incorporating professional-grade supplements, targeted nutrition, and lifestyle strategies to help you achieve vibrant health. Let’s embark on this journey towards a healthier, happier you!
Remember, a healthy gut is the foundation of a healthy life—take the first step today!
References:
1. Gut Microbiome and Diet:
- Wu, G. D., et al. (2011). "Linking long-term dietary patterns with gut microbial enterotypes." Science, 334(6052), 105-108. Retrieved from [Science Magazine]
- De Filippis, F., et al. (2016). "High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome." Gut, 65(11), 1812-1821. Retrieved from [Gut Journal]
2. Effects of Antibiotics on Gut Microbiome:
- Dethlefsen, L., et al. (2008). "The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing." PLoS Biology, 6(11), e280. Retrieved from [PLoS Biology]
3. Impact of Stress on Gut Health:
- Moloney, R. D., et al. (2014). "The microbiome: stress, health and disease." Molecular Neurobiology, 49(3), 736-756. Retrieved from [Springer]
4. Effect of Sleep on Gut Microbiome:
- Benedict, C., Vogel, H., Jonas, W., et al. (2016). "Gut microbiota and glucometabolic alterations in response to sleep loss in healthy individuals." Molecular Metabolism, 5(12), 1175-1186. Retrieved from [Molecular Metabolism]
5. Environmental Toxins and Gut Health:
- Järup, L. (2003). "Hazards of heavy metal contamination." British Medical Bulletin, 68(1), 167-182. Retrieved from [Oxford Academic]
6. Herbs and Gut Health:
- Scully, C., & Ettlin, D. A. (2017). "Herbs and Spices: Their Health Benefits and Risks." Journal of Clinical & Translational Endocrinology, 6, 74-82. Retrieved from [ScienceDirect]
7. Gut-Brain Axis and Emotional Well-being:
- Foster, J. A., & Neufeld, K. M. (2013). "Gut–brain axis: How the microbiome influences anxiety and depression." Trends in Neurosciences, 36(5), 305-312. Retrieved from [Trends in Neurosciences]
These references provide the scientific backing for the information discussed in the blog article, and you can visit these websites to explore the studies in detail.
Citations on related to gut bacteria:
1. Lactobacillus and Bifidobacterium:
- Klaenhammer, T. R., Altermann, E., Arigoni, F., et al. (2002). "Discovering lactic acid bacteria by genomics and proteomics: The Lactobacillus acidophilus group." Journal of Nutrition, 132(12), 2528-2530. [Oxford Academic]
2. Escherichia coli (E. coli), Clostridium difficile (C. diff), and Salmonella:
- "E. coli and Clostridium difficile in Gut Health." (2015). Centers for Disease Control and Prevention (CDC).[CDC] and [CDC]
3. Firmicutes and Bacteroidetes Ratio:
- Ley, R. E., Turnbaugh, P. J., Klein, S., & Gordon, J. I. (2006). "Microbial ecology: Human gut microbes associated with obesity." Nature, 444(7122), 1022-1023.[Nature]
4. Study Published in the Journal Nutrients:
- Makki, K., Deehan, E. C., Walter, J., & Bäckhed, F. (2018). "The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease." Nutrients, 10(10), 1205. [MDPI Nutrients]
Each of these sources provides detailed information about specific bacteria, their roles, and impacts on human gut health, as well as broader insights into the gut microbiome's influence on health and disease.
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾
Why the DUTCH Test is My Go-To Tool for Uncovering Hormonal Imbalances
As a Traditional Naturopath and Functional Diagnostic Nutrition® Practitioner, my mission is to help you achieve optimal health by addressing the root causes of your symptoms, rather than just treating them. One of the most powerful tools in my practice for understanding your body’s unique needs is the DUTCH test, a comprehensive hormone assessment that provides deep insights into your hormonal health.
Hormones are the body’s chemical messengers, playing a vital role in regulating everything from energy levels and mood to metabolism and reproductive health. When our hormones are balanced, we feel vibrant, healthy, and resilient. However, even small imbalances can lead to a range of issues, such as fatigue, weight gain, anxiety, sleep disturbances, and more.
The DUTCH test (Dried Urine Test for Comprehensive Hormones) offers a detailed view of your hormone levels and how they are metabolized in your body. This allows us to pinpoint imbalances and understand how they might be contributing to your symptoms. By gaining this level of insight, we can craft a personalized wellness plan that addresses your specific hormonal needs, helping you to restore balance and feel your best.
In this article, I'll explain why I use the DUTCH test in my practice, the incredible insights it provides, and how it can be the key to unlocking a healthier, more balanced you.
Why We Use DUTCH Testing: A Deep Dive into Hormonal Health
What is DUTCH Testing?
The DUTCH test is a cutting-edge diagnostic tool that measures hormone levels and their metabolites through dried urine samples. Unlike standard blood tests, which only provide a snapshot of hormone levels at a single point in time, DUTCH testing offers a more comprehensive view by assessing hormone production over a 24-hour period. This allows us to see not just the levels of hormones like cortisol, estrogen, progesterone, and testosterone, but also how these hormones are metabolized and excreted by the body.
Precision and Accuracy
The DUTCH test is known for its precision and accuracy. By using dried urine samples, it provides stable and reliable results, unlike single-point blood or saliva tests[1][2]. This accuracy is backed by peer-reviewed research, which validates the test's clinical utility and supports its use in both conventional and naturopathic practices[2].
Insights into Hormone Metabolism
One of the standout features of the DUTCH test is its ability to assess hormone metabolites. This insight is crucial for understanding how hormones are processed in the body, which can reveal potential imbalances or dysfunctions in hormone pathways[3][5]. Hormones play a crucial role in regulating various bodily functions, including mood, energy levels, metabolism, and reproductive health. Imbalances in these hormones can lead to a wide range of health issues, such as chronic fatigue, weight gain, anxiety, depression, infertility, and more.
The DUTCH test is particularly valuable because it provides a comprehensive analysis of several key areas:
1. Adrenal Function and Stress Response:
- The DUTCH test measures cortisol and cortisone levels throughout the day, offering insight into your body’s stress response. Chronic stress can lead to adrenal insufficiency, where the body struggles to produce sufficient cortisol, resulting in symptoms like fatigue, sleep disturbances, and weakened immune function.
- Research indicates that chronic stress and disrupted cortisol rhythms are linked to various health issues, including cardiovascular disease, obesity, and diabetes . By understanding your unique cortisol pattern, we can tailor interventions to support adrenal health and restore balance.
2. Sex Hormone Balance:
- DUTCH testing evaluates levels of estrogen, progesterone, and testosterone, along with their metabolites. This is crucial for identifying conditions like estrogen dominance, low progesterone, or low testosterone, which can contribute to symptoms like PMS, menopausal issues, infertility, and low libido.
- A study published in the Journal of Clinical Endocrinology & Metabolism highlights the importance of hormone metabolism in understanding conditions like estrogen-dependent cancers and endometriosis. DUTCH testing helps us see beyond hormone levels and understand how they are processed in your body, giving us deeper insights into potential health risks and how to address them.
3. Melatonin and Sleep Health:
- The test also assesses melatonin levels, a hormone crucial for regulating sleep-wake cycles. Disrupted melatonin production can lead to sleep issues, which in turn can affect overall health and well-being.
- Poor sleep is associated with numerous chronic conditions, including depression, anxiety, and impaired immune function. By evaluating melatonin levels, we can recommend natural interventions to improve sleep quality and support overall health.
4. Organic Acid Testing:
- DUTCH testing includes organic acid markers, which can give insights into neurotransmitter metabolism, nutrient deficiencies, and oxidative stress. This information is vital for understanding mood disorders, cognitive function, and overall metabolic health.
Men's Health Concerns: How DUTCH Testing Provides Key Insights
Men’s health concerns are often linked to hormonal imbalances that can significantly affect quality of life. The DUTCH test offers a comprehensive evaluation of androgens, including testosterone, DHEA-S (Dehydroepiandrosterone sulfate), and their metabolites, which are crucial for understanding various male health issues. Here’s how the DUTCH test helps address specific men’s health concerns:
1. Low Testosterone:
- Testosterone is a key hormone in men, responsible for muscle mass, bone density, mood regulation, and sexual function. Low levels of testosterone can lead to symptoms such as fatigue, depression, reduced libido, and loss of muscle mass. The DUTCH test not only measures total testosterone but also provides insights into free testosterone and its metabolites, offering a more complete picture of androgen status.
- This allows practitioners to identify whether low testosterone is due to poor production, excessive conversion into other hormones like estrogen, or issues with androgen receptor sensitivity. With this information, targeted therapies can be implemented to restore balance.
2. Abdominal Weight Gain:
- Hormonal imbalances are a common but often overlooked cause of abdominal weight gain in men. Elevated cortisol levels, as revealed through DUTCH testing, are linked to increased fat storage, particularly around the midsection. Additionally, imbalances in insulin, testosterone, and estrogen can contribute to weight gain and difficulty losing fat.
- The DUTCH test can help identify these imbalances, allowing for a comprehensive approach to weight management that might include stress reduction techniques, dietary changes, and specific supplements to support hormonal balance.
3. Gynecomastia (Male Breast Development):
- Gynecomastia, or the development of breast tissue in men, is often linked to an imbalance between estrogen and testosterone. The DUTCH test provides detailed information about estrogen levels and how well your body is metabolizing estrogen, offering insights into whether excess estrogen might be contributing to gynecomastia.
- By identifying issues such as poor estrogen metabolism or aromatase activity (the enzyme that converts testosterone into estrogen), practitioners can design a treatment plan to reduce estrogen levels and restore hormonal balance.
4. Male Pattern Baldness:
- Male pattern baldness is commonly associated with elevated levels of dihydrotestosterone (DHT), a potent androgen derived from testosterone. The DUTCH test measures not only testosterone but also its conversion into DHT, providing insight into whether this pathway is contributing to hair loss.
- Understanding these dynamics allows for more effective interventions, such as the use of natural DHT blockers, lifestyle modifications, or other targeted therapies to slow down or prevent further hair loss.
Comprehensive Insights for Tailored Solutions
The DUTCH test goes beyond standard hormone testing by offering a detailed analysis of how hormones are metabolized in the body. This is crucial because two men with the same testosterone levels might experience very different symptoms depending on how their body processes that hormone. The test also includes markers for adrenal function, which is important in understanding how stress impacts male hormones and overall health.
By gaining a comprehensive understanding of hormonal health through the DUTCH test, as your practitioner I can develop personalized treatment plans that address dietary adjustments, lifestyle changes, and targeted supplements, focusing on root causes of symptoms rather than just masking them. This leads to more effective and sustainable results, helping men and women restore hormonal balance and regain their vitality and well-being.
Fun Fact
A fun fact about Precision Analytical Inc., the creators of the DUTCH test, is that the company was founded by a scientist who wanted to create a more comprehensive and practical hormone testing method. Mark Newman, the founder of Precision Analytical, spent years working in hormone testing laboratories and noticed the limitations of traditional testing methods. He combined his extensive experience with a passion for innovation to develop the DUTCH test, which stands out for its ability to provide detailed insights into hormone metabolism using an easy, non-invasive collection method—just dried urine! This approach has revolutionized how practitioners assess and treat hormonal imbalances, making it more accessible and informative for both practitioners and patients.
Monitoring Treatment Progress
The DUTCH test is not just a diagnostic tool; it is also valuable for monitoring treatment progress. By regularly assessing hormone levels, I can track the effectiveness of interventions and make necessary adjustments to optimize outcomes[1][4]. This ongoing evaluation ensures that treatment plans remain aligned with the client's evolving needs.
The Precision and Depth of DUTCH Testing: Real Client Benefits
The beauty of DUTCH testing lies in its precision and the detailed data it provides. Here’s how it has helped our clients:
- Case Study 1: A client struggling with chronic fatigue and weight gain had normal blood cortisol levels. However, DUTCH testing revealed a flat cortisol curve, indicating adrenal dysfunction. With targeted adrenal support and lifestyle modifications, the client’s energy levels and weight normalized within months.
- Case Study 2: Another client experienced severe PMS and mood swings. Blood tests showed normal estrogen and progesterone levels, but DUTCH testing uncovered an imbalance in estrogen metabolism, leading to estrogen dominance. With dietary changes and herbal support, the client’s symptoms improved significantly.
DUTCH testing provides a wealth of data that helps in identifying the root causes of health challenges. For instance, it can reveal cortisol patterns that affect stress response and sleep, or estrogen metabolite ratios that may indicate a risk for estrogen-related conditions[3][4]. This information empowers clients to understand their hormone health better and engage in informed discussions about their treatment options.
Supporting DUTCH Testing
Numerous studies support the utility of comprehensive hormone testing in clinical practice. For example, a study in BMC Women's Health emphasized the importance of evaluating hormone metabolites in diagnosing and treating hormone-related conditions, particularly in women. Moreover, the ability to monitor cortisol patterns and sex hormone metabolism allows for a more nuanced understanding of how stress and hormones interplay in various health conditions.
Conclusion: Take Charge of Your Health with DUTCH Testing
If you’ve been struggling with unexplained symptoms, chronic fatigue, hormonal imbalances, or simply don’t feel like yourself, DUTCH testing could provide the answers you’ve been searching for. By identifying the root causes of your health challenges, we can create a customized wellness plan tailored to your unique needs.
Don’t wait for your symptoms to worsen or go untreated. Take the first step towards reclaiming your health today by scheduling a consultation. Together, we’ll uncover the imbalances holding you back and pave the way for lasting health and vitality.
Citations:
[1] https://londoncfm.co.uk/what-is-the-dutch-hormone-test/
[2] https://dutchtest.com/blog/responding-to-claims-in-a-recent-review-of-the-dutch-test/
[3] https://jilldumas.com/dutch-test-vital-hormones-hrt/
[4] https://integrative.ca/blog/dutch-complete-test-what-the-heck-is-it-and-how-can-it-help-me
[5] https://jilldumas.com/dutch-comprehensive-hormone-testing/
The information provided in the expanded section on men's health
Citations:
The information provided in the expanded section on men's health concerns related to DUTCH testing is primarily based on general knowledge of hormone physiology and the utility of DUTCH testing in clinical practice. Here are some specific citations and sources that align with the topics discussed:
1. Low Testosterone:
- The role of testosterone in men's health and its impact on various physiological functions is well-documented in clinical literature. For more detailed information on the role of testosterone and the benefits of comprehensive testing:
- Travison, T. G., Araujo, A. B., O'Donnell, A. B., Kupelian, V., & McKinlay, J. B. (2007). A population-level decline in serum testosterone levels in American men. The Journal of Clinical Endocrinology & Metabolism, 92(1), 196-202. [Link to study](https://academic.oup.com/jcem/article/92/1/196/2598066)
2. Abdominal Weight Gain:
- The link between cortisol, insulin resistance, and abdominal weight gain is supported by numerous studies. High cortisol levels, often due to chronic stress, are associated with increased abdominal fat:
- Bjorntorp, P. (1991). Metabolic implications of body fat distribution. Diabetes Care, 14(12), 1132-1143. [Link to study](https://diabetesjournals.org/care/article/14/12/1132/19684/Metabolic-implications-of-body-fat-distribution)
- Pasquali, R., Vicennati, V., Cacciari, M., & Pagotto, U. (2006). The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Annals of the New York Academy of Sciences, 1083(1), 111-128. [Link to study](https://pubmed.ncbi.nlm.nih.gov/17148733/)
3. Gynecomastia (Male Breast Development):
- Gynecomastia's connection to hormone imbalances, particularly the ratio between estrogen and testosterone, is well understood in endocrinology:
- Carlson, H. E. (2011). Gynecomastia. The New England Journal of Medicine, 365(19), 1827-1835. [Link to study](https://www.nejm.org/doi/full/10.1056/nejmcp1013710)
- Johnson, R. E., & Murad, M. H. (2009). Gynecomastia: Pathophysiology, evaluation, and management. Mayo Clinic Proceedings, 84(11), 1010-1015. [Link to study](https://pubmed.ncbi.nlm.nih.gov/19880694/)
4. Male Pattern Baldness:
- The association between dihydrotestosterone (DHT) and male pattern baldness is widely recognized in dermatology and endocrinology:
- Sawaya, M. E., & Shapiro, J. (2000). Androgenetic alopecia: New approved and unapproved treatments. Dermatologic Clinics, 18(1), 47-61. [Link to study](https://pubmed.ncbi.nlm.nih.gov/10669597/)
- Trueb, R. M. (2002). Molecular mechanisms of androgenetic alopecia. Experimental Gerontology, 37(8-9), 981-990. [Link to study](https://pubmed.ncbi.nlm.nih.gov/12175493/)
These references provide scientific support for the topics discussed in the expanded section on men’s health concerns and how DUTCH testing can help address these issues.
Here are more sources and citations used for the information in the blog article:
1. Cortisol and Adrenal Function:
- Chronic stress and its impact on health are widely studied. The connection between stress, cortisol rhythms, and health issues like cardiovascular disease and diabetes is well-documented in sources like:
- Nater, U. M., & Rohleder, N. (2009). Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology, 34(4), 486-496. [Link to study](https://pubmed.ncbi.nlm.nih.gov/19155141/)
- Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7), 374-381. [Link to study](https://pubmed.ncbi.nlm.nih.gov/19488073/)
2. Sex Hormone Balance and Metabolism:
- The importance of hormone metabolism in understanding conditions like estrogen-dependent cancers and endometriosis can be referenced from:
- Ziegler, E. E., & Filer, L. J. (1996). Estrogens and progestogens: health risks and benefits. The Journal of Clinical Endocrinology & Metabolism, 81(11), 3864-3871. [Link to study](https://academic.oup.com/jcem/article/81/11/3864/2875096)
- Kaaks, R., & Lukanova, A. (2001). Energy balance and cancer: the role of sex hormones. Proceedings of the Nutrition Society, 60(1), 51-64. [Link to study](https://pubmed.ncbi.nlm.nih.gov/11310428/)
3. Melatonin and Sleep Health:
- The relationship between melatonin, sleep quality, and health issues such as depression and anxiety is explored in:
- Medic, G., Wille, M., & Hemels, M. E. H. (2017). Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep, 9, 151-161. [Link to study](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5449130/)
- Wright, K. P., Jr., & Lack, L. C. (2001). Effect of light exposure on melatonin and subjective sleepiness in humans. Sleep, 24(4), 403-411. [Link to study](https://pubmed.ncbi.nlm.nih.gov/11403527/)
4. Hormone Metabolites and Women's Health:
- The relevance of hormone metabolites in diagnosing hormone-related conditions, particularly in women, is discussed in:
- Riecher-Rössler, A., & Häfner, H. (2000). Gender aspects in schizophrenia: bridging the border between social and biological psychiatry. Acta Psychiatrica Scandinavica, 102, 58-62. [Link to study](https://pubmed.ncbi.nlm.nih.gov/11321222/)
- BMC Women's Health. (2021). [Link to study](https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-023-02319-x)
These references provide a scientific foundation for the benefits and applications of DUTCH testing in assessing hormonal health, stress response, and overall well-being.
DISCLAIMER: The health information in this blog are for general education and is not intended to substitute for any medical advice. No medical cure, diagnosis, or treatment is provided.
This website contains affiliate links, which means LTL may receive a percentage of any product or service you purchase using the links in the items descriptions, articles or advertisements. You will pay the same price for all products and services, and your purchase helps support our ongoing effort in assisting you. Thanks for your support!
✨ Unlock expert wellness insights! 🌿 Subscribe now for exclusive health tips & natural living secrets! 🌱💪🏾